NHSE's operating model and oversight framework aim to clarify the role of ICBs in the new context of system working, positioning them as the first line of oversight and performance management of trusts. The Hewitt Review also reflected on the role and responsibilities of ICBs, reemphasising the principles of the two frameworks and the importance of subsidiarity and effective co-design.
In our conversations with NHSE, and in our commentary on the Hewitt Review, we have highlighted the inherent tension in ICBs being positioned as convenors and equal partners within their systems, and in overseeing performance. We have identified the challenging position this puts both trusts and ICBs in, and the potential for conflicts of interest.
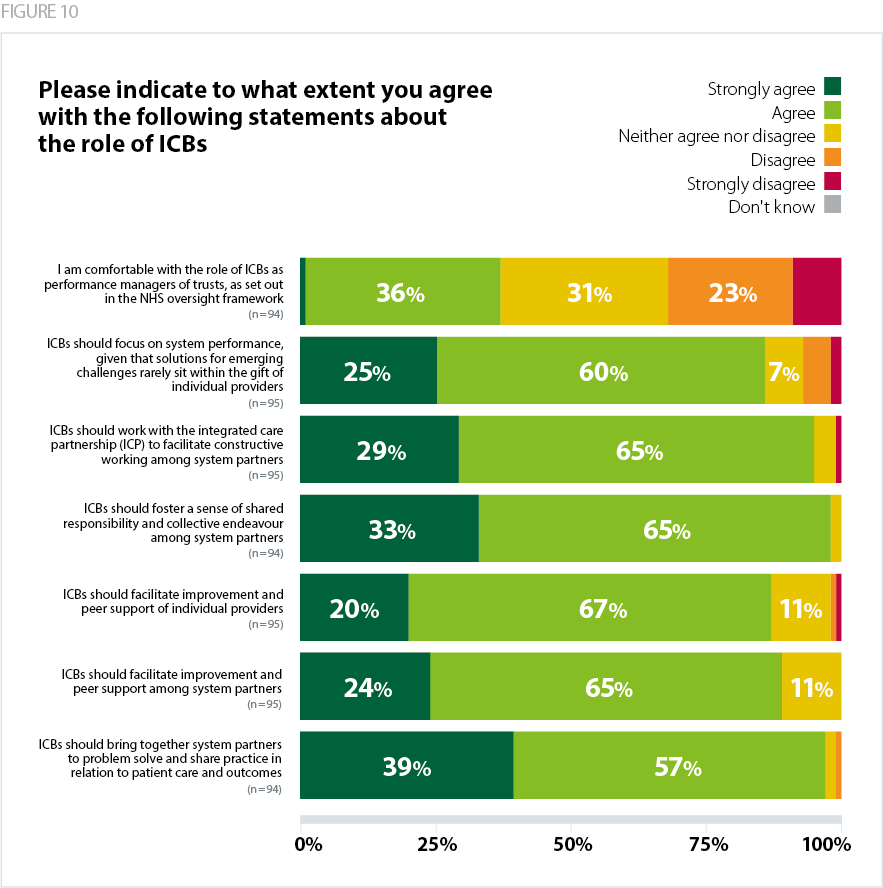
Figure 10 below reveals overwhelming support from trust leaders for ICBs’ role in fostering a sense of shared responsibility and collective endeavour among system partners (98% agreed), as well as in bringing system partners together to solve problems and share practice on patient care and outcomes (96% agreed). Trusts were also very supportive of ICBs’ constructive work with ICPs (94% agreed), their role in improvement and peer support (89% agreed), and their focus on system performance (85% agreed).
Views were markedly split on the role of ICBs as performance managers of trusts: only 37% were comfortable with this role, while just under a third (32%) disagreed. Acute trusts were the most sceptical, with 44% disagreeing.
While supportive of the aims of ICBs, many respondents said that it was too early to assess their impact and highlighted variable maturity across systems.
"They remain too early in their development to draw strong views on"
"Some ICBs are more mature than others. Some haven't settled on effective governance yet."
Several comments highlighted confusion and lack of clarity around the role of ICBs, with some saying that ICB leaders themselves were unclear.
"It is early days but we are still very confused about the role of ICBs. If ICBs are to do performance management they are too small in the [REGION] and do not have the skills and governance in place to do this effectively."
Our ICB leaders are confused. They don’t see themselves or want to be performance managers but NHSE are pushing that. They are too wrapped up in making the governance look shiny, reducing headcount and preparing for delegation of services to be interested in anything else. We do not have the right
ICB leaders... They simply cannot do it.
Several respondents pointed out the importance of culture and behaviours.
"ICBs function differently due to different behaviours and approach; therefore it’s more about the culture based on past experience."
A large number of comments reflected views on the optimal role for ICBs – there was a strong feeling that ICBs should focus on collaboration across a system.
"I feel strongly that ICBs should play a key role in bringing about strong, constructive collaborative working across the system, including working with individual partners to improve performance. Locally, we are nowhere near there yet - there is still far too much jockeying for advantage…"
There was scepticism around the role of the ICB as performance manager.
"It is too early to say if the changes will clarify and improve the role of ICB but I am concerned that mixing performance/oversight with system-wide partnership development is incompatible. It requires the ICB to play two roles which could be in conflict."
"ICBs must not duplicate the performance management and oversight which is already embedded and proportionate in trusts."
"ICBs' role in performance management needs to be focussed at system rather than individual providers to avoid duplication. There remains tension between statutory provider boards and ICB board committees."
A couple of respondents pointed out the potential of provider collaboratives to improve system working, based on their current experience.
"My experience is that ICBs are still trying to resolve internal appointments and have yet to start in earnest, while grappling with major deficits. Their potential for improved system working is as yet untapped. By contrast, one of our provider collaboratives (for acute and specialist services) is effective in filling some of the gap for system working."
The introduction of ICBs was often associated with an increased burden, while the confusion and duplication between NHSE and ICBs was highlighted multiple times. Some trust leaders reported that requests from ICBs had been more onerous than those coming from the regulators themselves.
“The requests for information from NHSE [are] suffocating and they now include ICBs in this so we are now asked for the same thing on multiple occasions. Even worse, the ICB request from executives but their managers then go directly to our managers so the request is coming like a scattergun and in the end no one knows who is doing what."
"Still very confused between ICB and NHSE - duplication abounds. Lots of people asking similar questions with slightly different requirements - needs streamlining!"
"It has been the requests from the ICB that have at times becomes onerous rather than those from NHSE or CQC and with limited usefulness."