

In this February edition we explore the activity and performance of trusts across mental health, community, ambulance and acute sectors. We also take a detailed look at winter pressures.
Progress in shrinking the elective and diagnostic waiting lists continued this month. This remains a key priority for the government, as signalled by the publication of its strategy for Reforming elective care for patients. Our On the Day Briefing provides an overview of the plan and our view. Long waits across other services need equivalent focus. It is vital that the 10-year plan addresses backlogs in other sectors including those in community and mental health services.
Capacity pressures facing trusts has been the central theme throughout the data released by NHS England (NHSE) in February. The winter data highlights very high adult bed occupancy in acute trusts, with this challenge being compounded by discharge delays and patient flow issues across the system.
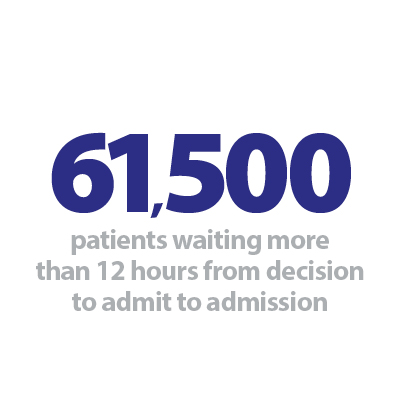
Monthly A&E data speaks to this picture of stretched capacity too, with a record number of patients waiting more than 12 hours from decision to admit to admission this month. However, improvements were observed for the ambulance sector with reductions in category 1 and 2 response times.
Trust leaders and staff continue to do everything they can to see patients as quickly as possible in the face of extreme pressure and challenges. Nevertheless, capacity is a whole system issue, and the unrelenting pressures are being mirrored in the community and mental health sectors too.
Community waiting lists increased and the number of patients in contact with mental health services was recorded above 2 million for the first time. The latest data also highlights that children and young people are being heavily impacted by long waits across mental health and community services.
Trusts are working to drive improvements across the system, and this month our case study spotlights positive changes to ambulance services and mental health crisis care that have been implemented across trusts in Greater Manchester.
Case study
On the road to better mental health crisis care
Danielle Lord, service manager at Pennine Care NHS Foundation Trust discusses how new mental health response vehicles are improving mental health crisis care across Greater Manchester.
Across Greater Manchester, nearly 600 people have been supported by new mental health response vehicles – with 453 avoiding A&E (77%).
The vehicles are run by North West Ambulance Service NHS Trust (NWAS) alongside Pennine Care and Greater Manchester Mental Health NHS foundation trusts, which provide mental health and other services across Greater Manchester.
For all ages, it involves an emergency medical technician from NWAS and a mental health practitioner from Pennine Care or Greater Manchester Mental Health jointly responding to 999 NWAS calls where the person is experiencing a mental health crisis. Some may also have a physical health need.
The patient can be treated at the scene, or signposted to an appropriate community-based service, instead of going to A&E which isn't the best place for most people.
Making sure they quickly receive the right care, in the right place, will benefit their recovery, ensure they have a positive experience and make best use of professionals' time.
An added bonus is that the vehicles are electric, in line with the national greener NHS programme to achieve net zero carbon.
Together we can provide the right mental health care, in the right place.
We've made many improvements to mental health services over the last couple of years. We'll continue to work hard with our partners to transform services and ensure a happier and more hopeful life for everyone in our communities.
Summer Kumar, mental health liaison lead at NWAS, added: "We're working closely with partners to meet the aims of the NHS long-term plan for those in a mental health crisis. We look forward to seeing more positive outcomes for people who need us."
Debbie Robinson, strategic lead for urgent and emergency care at Greater Manchester Mental Health, said: "We're delighted to be working in partnership to deliver this important service for our communities.
"Being able to treat people experiencing a mental health crisis directly at the scene is better for the patient's recovery and our mental health practitioners can make referrals to relevant services quickly and more effectively."
For more information visit: www.penninecare.nhs.uk/mental-health-response-vehicle-launch