
Week seven of the winter sitreps brought mixed news today, as bed occupancy remains extremely high but other indicators saw improvement on the previous week. The latest NHS workforce figures and sickness absence rates were also released, providing additional insight to the current conditions in trusts across the country.
A headline bed occupancy level of 95.0% shows just how stretched the system is and, following on from an even higher figure last week, there is concern that this will become entrenched for the rest of the winter. On the positive side, trusts did not have as many escalation beds open this week, and there were fewer ambulance arrivals, a reduction in beds closed with D&V and norovirus and fewer long-stay patients compared to week six. While the NHS workforce figures released today for October 2019 show growth in total staff numbers from the previous month and a healthy increase in the past year, sickness absence rates also released today for September 2019 have never been higher at this time of year.
Key week seven sitreps headlines:
- bed occupancy is 95.0%, still extremely high and only a miniscule reduction from 95.1% last week
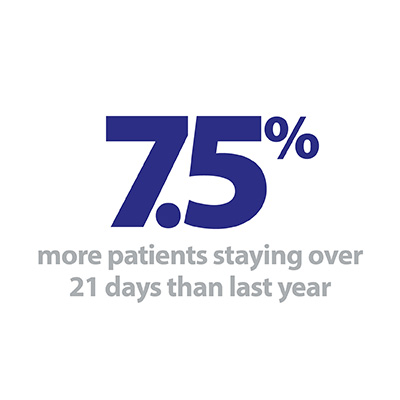
- length of stays are slightly better than last week, but still much higher than last year
- total beds open fell by 0.2% this week, and escalation beds were down by 6.7% (300 fewer)
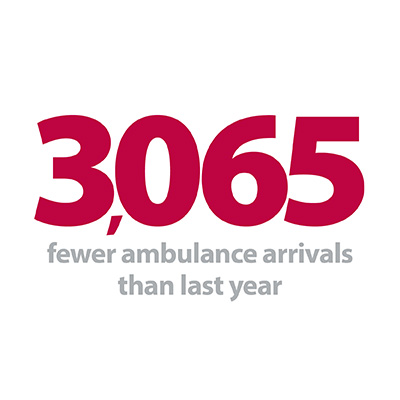
- ambulance arrivals are down by 1,226 on last week (-1.3%)
- ambulance handovers are better than last week, but still higher than last year.
Other new data released today:
- total NHS workforce in October 2019 was 0.7% higher than the previous month, and 3.6% higher than the same time last year
- the sickness absence rate for September 2019 was 4.25%, the highest it has ever been at this time of year.
This week, there were reductions in the number of patients staying in hospital longer than 7, 14 and 21 days, although these all remain higher than at any point last winter. Efforts to send patients home, or to more appropriate care settings as they recover are as important as ever, both for the individual and trust. Delayed transfers can have a knock-on effect in a number of ways, and shortages and sickness absence in key workforce groups are determining factors in how quickly patients can be discharged.
Fewer patients arrived by ambulance this week, with the week seven total of 94,512 a reduction of 6.3% on the highpoint reached in week three, or 910 fewer arrivals per day.
Fewer patients arrived by ambulance this week, with the week seven total of 94,512 a reduction of 6.3% on the highpoint reached in week three, or 910 fewer arrivals per day. Correspondingly, a smaller proportion of arrivals were delayed this week, with 13.1% waiting 30 minutes or longer, down from 16.3% in the previous week. This still equates to over 12,000 patients being delayed at a crucial moment in their care, and trusts continue to seek innovative ways to smooth the flow of patients arriving by ambulance in settings already at maximum capacity.
Beds closed with D&V and norovirus fell this week, but with relatively mild weather this was not a huge surprise. Fears remain that a cold snap could result in a rise in flu, D&V and norovirus, and trusts will additionally be monitoring the troubling spread and prevalence of coronavirus in the coming weeks.
Winter pressures on the frontline: A doctor's explanation to patients
Dr Jen Rhodes, an emergency medicine consultant at the Queen Elizabeth Hospital, run by Gateshead Health NHS Foundation Trust, discusses winter pressures on frontline services and how a triaging service is helping staff to manage demand.
Like many other trusts across the country, Gateshead faces significant pressure from an increase in demand over the winter months. Dr Rhodes highlights how seasonal conditions contribute to the problem, including outbreaks of flu and norovirus, and more attendances following falls due to icy conditions. Over winter the department also attends to more elderly and frail patients who are more prone to becoming unwell, and who may have more complex treatment needs or multiple health conditions.
Frontline staff are working flat out to ensure that patients are kept safe and various teams in the emergency department are working effectively together to deliver high-standard care.
Patients are brought into the emergency department either by ambulance or walk-in. Dr Rhodes describes the triage procedure that all patients experience upon arrival to prioritise those with the most urgent medical needs. This helps maintain patient safety, but may mean that those well enough may wait longer for treatment. The triage also helps ensure that the patient is seen by the most appropriate clinician - usually either a GP, doctor or nurse.
Dr Rhodes explains that patients can also help reduce the pressure on services by accessing medical treatment or advice from elsewhere over winter if appropriate and their condition is not an emergency. This may mean visiting a GP or pharmacy, using the NHS website or calling 111 for advice, or attending an urgent care centre.
Little breathing space for trusts amid winter pressures
Responding to the latest weekly winter reporting data published by NHS England and NHS Improvement, and the latest NHS workforce statistics, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"It is clear that there is little breathing space for trusts as they continue to work flat out to manage winter pressures.
"While we have seen 1,200 fewer ambulance arrivals and a reduction in handover delays this week, more people are waiting longer to be seen when they arrive in a hospital than at this time last year.
"These delays, which leave patients waiting in ambulances or corridors to be admitted, are a symptom of blockages in the rest of the system. Bed occupancy remains extremely high, despite the best efforts of staff to get patients home or into the community as soon as is appropriate.
"While we have seen the NHS workforce grow by 3.6% overall in the past year, burn out among staff is evident with the latest sickness rates being the worst on record for the time of year. There is no question that staff are going above and beyond to deliver high-quality care and keep patients safe amid rising demand, but ultimately staff shortages reduce the services available and will lead to longer waits for patients.
"We need to break the cycle of winter pressures, ensuring the whole health and care system can meet growing demand by investing in community and social care, looking after the NHS workforce, and continuing to support joined-up working between services."