
Today we saw the sixth week of the winter sitreps published by NHS England and NHS Improvement. Although COVID-19 cases seem to be decreasing, we are still seeing high levels of hospital admissions and patients in hospital. Recent data (11 January 2022) show a decrease of 30% in the number of cases since the week before, yet the number of hospital admissions on 9 January was up by 5% since the week before and the number of patients in hospital on 11 January was up by 13%. Therefore, it is likely to be some weeks until we see the decline in cases reduce COVID-19 related hospital activity. Additionally, the number of staff absences remains considerably high, having increased from the week before, with over half of the absences being COVID-19 related (45,736).
In addition to winter sitrep data, the monthly NHS performance and activity figures were also released today, providing useful context to the state of the sector heading into January and prior to the Omicron wave.
Key points to highlight include:
A&E: December saw 1.8 million attendances, a decrease of 8% from November yet still higher than one year ago (+27%). Emergency admissions were slightly up from the last month but also 8% higher than one year ago. Concerningly, the number of patients waiting more than 12 hours from the decision to admit to admission has increased by a fifth on the previous month to 12,986 (the highest number on record). The number has tripled in a year (an increase of 246% since last December) and is over five times greater than two years ago before the pandemic.
NHS 111 and ambulance: unlike A&E attendances, there was an increase in the number of NHS 111 calls received, and category 1 incidents registered the highest figure on record (34% greater than the same time last year). Both category 1 and category 2 average response time targets were missed again in December.
Elective care: the size of the waiting list has increased again to almost 6 million in November, now being 36% greater than two years ago before the pandemic. That said, the number of admitted inpatient pathways, non-admitted pathways and new referral to treatment pathways all increased from the previous month.
Cancer: in November record numbers of patients have been seen by a consultant following an urgent two-week GP referral. Even though performance against the waiting time standards fell slightly across all pathways, all activity has increased from the previous month.
Diagnostics: diagnostic activity continued to increase in November and reached similar levels to before the pandemic. That said, the waiting list also increased and was at an all-time high (1,455,012).
Mixed-sex accommodation (MSA) breaches: the number of MSA breaches in November has increased by 7.5% to 2,586 since the previous month (181 more). This is much lower than the peak at the start of the pandemic (47.5% lower than February 2020) but is 31.4% higher than pre-pandemic levels (618 more breaches than November 2019).
Looking at the weekly sitrep figures, they highlight the current challenges with ambulance handover delays still higher than one year ago, both general and acute (G&A) and critical care bed occupancy rates climbing again this week, and more patients staying longer than seven, 14 and 21 days. These are the key figures from week six:
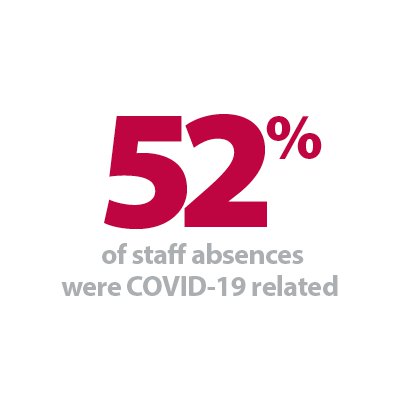
- There was an average of 88,516 staff absences this week (8,221 more), of which over half (52%) were due to COVID-19 (45,736). Total absences increased by 10% since last week (week 5), whereas COVID-19 absences increased by 28%. However, COVID-19 absences are 81% higher than week 4 (20-24 December).
- An average of 94,617 G&A beds were open this week, representing an occupancy rate of 91.8% (up from 88.5% last week). This is a particularly concerning figure, due to the additional demands of COVID-19 pathways and the ongoing Omicron variant wave.
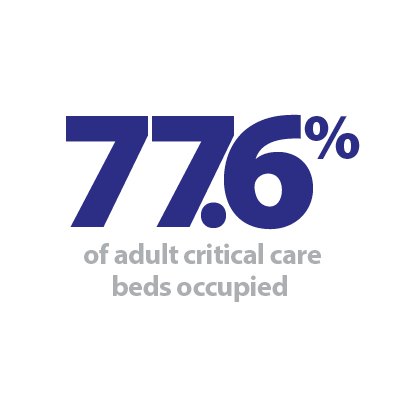
- Adult critical care bed occupancy has increased since last week to 77.6%. However, this is lower than the same time last year (83.4%).
- A total of 81,129 patients arrived by ambulance this week. This is a decrease of 3% since last week (2,511 fewer) and lower than the same time last year (5.7% or 4,927 fewer arrivals). Ambulance handover delays fell slightly this week with 22.6% of ambulance handover delays being delayed by 30 minutes or more (down from 22.8% last week) and 9.8% being delayed by 60 minutes or more (down from 9.9% last week). Both figures are considerably higher than the same time last year.
- The number of beds closed due to diarrhoea and vomiting and norovirus has dropped considerably by 43.6% this week and is at its lowest level since the start of this winter's sitreps (106), although it is still higher than this time last year (76). Conversely, the number of G&A beds occupied by flu patients increased by 23.3% to 318 (60 more). A total of 19 critical care beds were occupied by flu patients this week (8 more).
- On 9 January there were 17,303 patients who no longer met the criteria to reside in hospital in the latest week. Of these, 12,396 (72%) remained in hospital.
- There were more patients staying longer than seven, 14 and 21 days this week, with these figures all rising from last week, as well as increasing from the same time last year (up by 18.7%, 27.6% and 34.8%, respectively).
On this sixth week of our Winter Watch campaign, these data continue to highlight how remarkably busy the NHS is at the moment. Trusts are facing ongoing seasonal pressures, COVID-19 care needs, the delivery of a rapid vaccination programme all alongside increased demand.
The latest activity data reflect how focused trusts were on care backlog recovery before the Omicron variant emerged. There were record numbers of cancer patients seen by a consultant following an urgent GP referral, greater levels of impatient elective activity and increased diagnostic testing.
In December, however, alongside the spread of Omicron, category 1 ambulance incidents reached a record high, A&E attendances and emergency admissions were higher than one year ago, and those waiting 12 hours or more to be admitted increased by a fifth on the previous month. These data show real pressure across the emergency care pathway and reflect the ongoing efforts of NHS staff, against the backdrop of huge staff absences.
The winter sitrep data highlight current challenges, with ambulance handover delays still higher than one year ago and more patients staying longer than seven, 14 and 21 days. Equally, the number of beds occupied, both G&A and in adult critical care wards, are concerning, particularly as we are also seeing an increasing number of delayed discharges. High staff absences caused by COVID-19 are a stark reminder of the virus' impact on the workforce.
Trusts undoubtedly still have challenging times ahead in relation to the Omicron variant, and trust leaders are rightfully concerned about its strain on their already busy services.
The Provider Podcast - Winter Watch : Omicron and Winter Pressures
As part of The Provider Podcast, NHS Providers director of communications Adam Brimelow, invites NHS Providers' chief executive Chris Hopson, deputy chief executive Saffron Cordery, and senior research analyst Luís Costa da Silva, to assess the impact of Omicron and the latest statistics indicating how the NHS is handling winter pressures.
Postponing of inspections over the winter period to support services
Care Quality Commission (CQC) chief inspector of hospitals, Professor Ted Baker, discusses the organisation's approach to regulation during the COVID-19 pandemic, and how they are supporting services by postponing inspections during this challenging time.
I am pleased to have the opportunity to write a blog for this year's Winter Watch campaign. I want to firstly use this opportunity to acknowledge the enormous efforts of health and social care staff – both frontline and leadership – throughout another phenomenally challenging year. Across the country, the resolve and tenacity of staff has kept the health and social care system running, keeping people safe wherever possible. We owe a huge amount to you all.
At CQC we have kept our approach under review since the start of the pandemic, adapting to the changing situation and making fast-paced decisions where necessary. In December we announced that we would be postponing inspections, following the government decision to accelerate the vaccine booster programme in response to new data about the spread of the Omicron variant. It was clear how much additional pressure this would put on already stretched services, leading us to make the decision to pause on-site inspection activity in all services involved in supporting the booster programme – except in cases where we have evidence of risk to life, or the immediate risk of serious harm to people. This will remain our approach for the time being.
We want to do all that we can to support services during this time, including working within our powers to increase capacity across the system. In adult social care this includes an ambition to complete 1,000 infection prevention and control inspections and respond rapidly to requests to set up new designated settings. From this month, we will begin a programme of activity to support the creating of additional capacity, including rating adult social care services that are registered and not yet rated, and inspecting those currently rated as 'requires improvement' to identify improvement where it has been made and update ratings where necessary. We hope that all of these actions will help with discharging people from other settings, including very busy urgent and emergency care units, and will ease the pressure on individual providers by fully utilising services across the system.
The increasing number of Omicron cases has put services under intense pressure, exacerbated by staff sickness due to COVID-19, and we recognise that normal expectations for staffing levels cannot always be maintained. We will support providers that are taking balanced, risk-based decisions in partnership with people who use health and social care to maintain access to services and keep them as safe as possible in response to system pressures.
Throughout the pandemic we have seen innovative practice despite the challenging circumstances under which services are operating. We are making a concerted effort to highlight this in our communications, including in our inspection reports and press releases. We know that even when a service is not performing at the highest level there is still a remarkable amount of hard work and good practice taking place thanks to the commitment and determination of staff.
As we move through the winter months the situation will continue to be difficult and services will struggle, but we recognise that we are all working towards the same goal – to keep people safe. Patients are at the heart of what we all do, and we will continue to work with providers and partners across the system to support services and staff, create capacity, and ultimately ensure people are receiving the best care possible during an incredibly tough period. I hope that you will also work with us by talking to your local inspection teams about the difficult decisions you are facing, so that we can support you and work together wherever possible.
NHS figures demonstrate intense pressures trusts are under
Responding to the latest monthly combined performance data, and the latest week of winter reporting data, from NHS England and NHS Improvement, the deputy chief executive of NHS Providers, Saffron Cordery said:
"These figures demonstrate the intense pressure trusts are under, and the incredible work NHS staff are doing to deliver care.
"We continue to be deeply concerned by the strain across urgent and emergency care, with the highest number of category 1 ambulance calls on record and an increase in the those waiting 12 hours or more for admission in emergency departments.
"There has also been a worrying increase in the number of beds occupied, remaining at a very high level, including in adult critical care wards.
"At the same time, the number of delayed discharges continues to grow, given the limitations on capacity in social care as some care homes had to reduce new admissions due to the rise of Omicron.
"These figures also highlight the extraordinary work being undertaken by NHS staff, including before the Omicron surge to address long waiting lists. There has also been a record number of urgent cancer referrals in November, and the highest amount of diagnostic activity since January 2020.
"This is all taking place in a context of increasing staff absences, which have grown by a further 10% this week and of which half were due to COVID-19. The fact that these absences are across all regions in England reflects how Omicron is moving beyond the epicentre in London."