Some trusts expressed concerns that services may not return to a level patients are treated as quickly as they would like, and expressed a need for nuance in conversations between government and the national bodies, and with the public, about which services would resume, and when.
They estimate that on average, they are operating at 53% capacity for non-COVID services, anticipating a rise to 70% in three months time, and 83% within six to 12 months. Again, ambulance trusts and mental health trusts estimate their current level of capacity to be higher than the acute sector (97% and 87%, rising to 100% and 99% respectively). Community trusts and acute trusts have lower current capacity (43% and 53%, rising to 77% and 88% within 6-12 months).
Trusts are clear that they have continued to offer services where they can and are confident that they can meet the needs of all patients who have urgent requirements. However, while some services will be able to resume quickly, particularly with the continuation of remote and digital care, many respondents conceded that services were unlikely to return to a level comparable to before the pandemic, for all patients as capacity is necessarily reduced due to the need for social distancing, PPE and infection control requirements, keeping COVID-19 and non-COVID patients apart, and the need to retain surge capacity within the system to guard against future potential spikes of the virus:
- trusts emphasised the need to prioritise at this stage of their planning: 80% said they are prioritising patients according to urgency
- across all trust types, just over a third (36%) said they have stopped accepting non-urgent referrals for a period of time - significantly smaller numbers of mental health trusts and ambulance trusts have done this (8% and 0% respectively), reflective of the differential needs of the people using their services, and their different roles in the response to the coronavirus
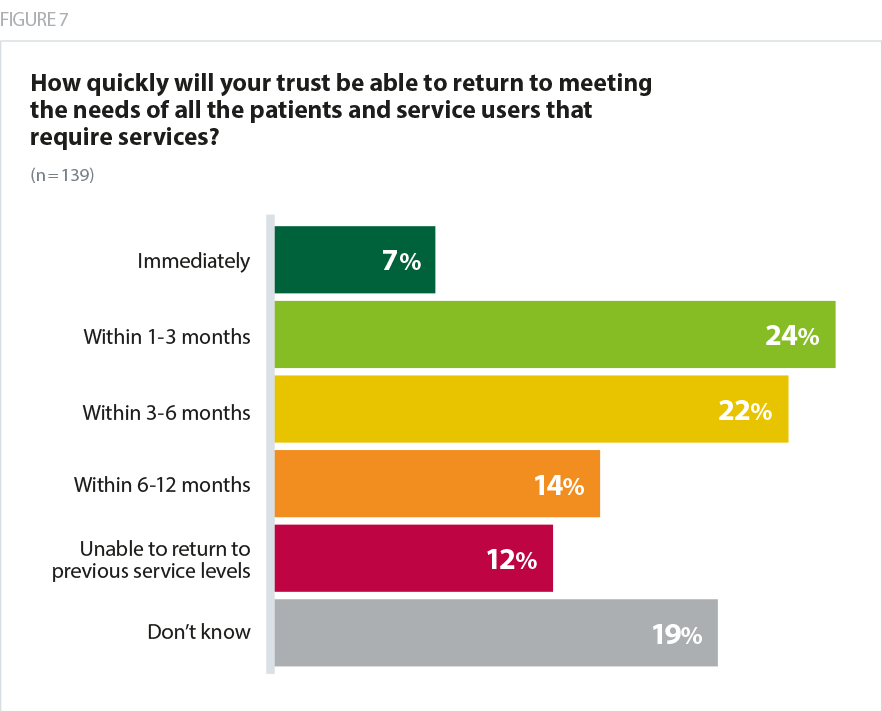
- when asked how quickly their trust would be able to return to meeting the needs of all patients, just 7% felt that their trust would be able to immediately return to a full level of service. Around a quarter (24%) said they could return to meeting all patients’ needs in 1-3 months and a further 22% said it would take 3-6 months, taking trusts into the autumn with substantial ramifications for winter planning.
COVID-19 will have impacted inequalities further and many of the vulnerable, at risk groups may not seek care and will be socially isolated and economically impacted. The NHS' recovery needs to prioritise resources to the invisible patients… and this is a good opportunity to reframe what our priorities are.
combined acute and community trust
I am confident that we will meet the needs of all patients who have urgent requirements. But such is the backlog I suspect it will take us to the end of the year to clear the backlog before taking new routine referrals.
combined acute and community trust
Respondents named a number of factors they need to take into account as they plan the return of services; one pointed out that in surgical theatres, there are now 20 minute waiting periods before and after intubation and between patients, reducing capacity by one hour per patient. Others are factoring in winter planning, pressures on social care and other services. Mental health trusts are factoring in a new and unknown level of mental health need as a result of the outbreak on top of existing demand. Ambulance services have to pause to deep clean vehicles after a suspected COVID case, however it is clear that it is acute trusts facing the greatest difficulties in restoring services quickly.
We will not be able to do major elective procedures anytime soon as COVID-19 is having a significant impact on productivity in theatres and bed spaces are significantly reduced with required social distancing.
acute trust
I am concerned that we may not have the staffing capacity to resume business as usual alongside the additional workload we have taken on in relation to supporting shielded patients, supporting recovering COVID patients in the community post discharge. We will look to new ways of working including use of technology to increase our productivity but that may not be sufficient.
community trust
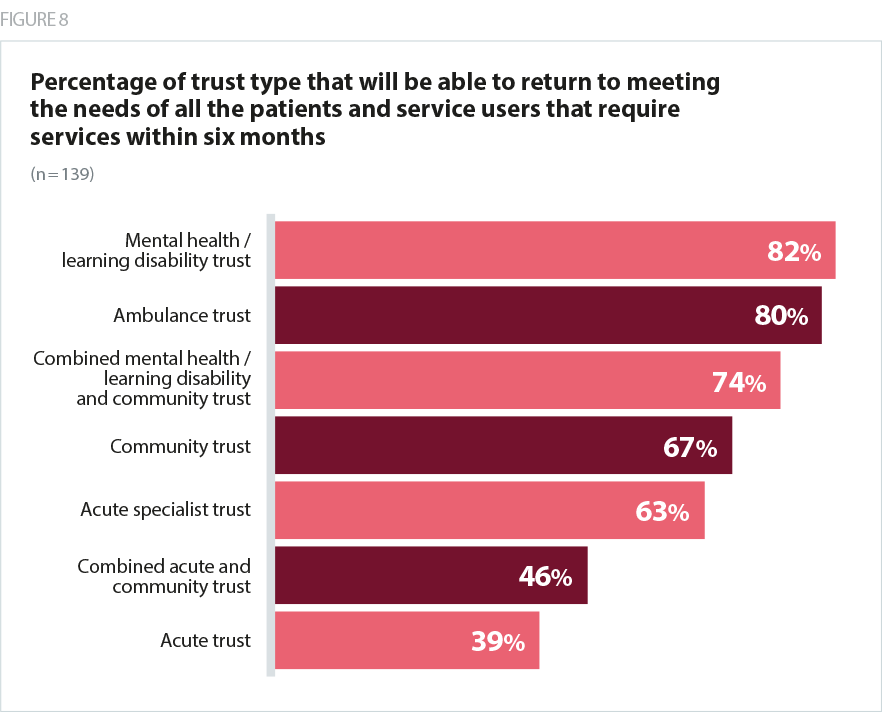
A small number of respondents (12%) said that their trust would not be able to return to its previous level of service. This varied considerably by sector, reflecting the differential impact the pandemic has had on different types of services:
- a quarter of specialist trusts and a fifth of acute trusts said they would not be able to return to their previous level of service, but none of the community, mental health or combined community and mental health trusts responding felt this would be the case for their trust
- Ttust leaders emphasised the challenge inherent in responding to this question with any degree of certainty - a fifth could not give any indication about how long it would take to return to their trust’s previous level of services, and while trust boards are carrying out detailed work to model how quickly they can resume normal services, with some already up and running remotely with social distancing in place, it’s clear there is a substantial level of uncertainty to contend with
- there is variation between sectors, with 40% of ambulance trusts saying they will return to full capacity immediately.
We have continued throughout to deal with the demands on service that have presented through 111, 999 and clinical assessment. The ambulance sector has never been in a stronger position in terms of performance and this is a strong indicator that when the sector is adequately resourced to meet demand it can heavily influence the success across other elements of pathways for patients.
ambulance trust
There is also some regional variation, with trusts in London more likely to feel confident in returning to a normal level of service immediately (16%) compared to the midlands (0%) and the North West (0%). This underscores the need for a regional approach to restoring services in reflection of the different pace at which the COVID-19 outbreak has progressed across the country. Areas with fewer active cases are more likely to be able to arrive at a new normal way of working than those with ongoing virus spread and existing high pressure on COVID-19 areas, but remain vulnerable to further spikes in cases.
Here in [south coast] we are clearly likely to have several surges because of summer visitors. Hotels are currently reporting up to 80% bookings for July and August, and holiday rentals up to 100%. The issue here is that the visitors may not be ill but be carriers and there is little indigenous immunity in [south coast] as our numbers have been relatively low to date. So we are preparing to bring more services on line relatively fast, using our different sites for trauma and orthopaedics, COVID and non-COVID and ED on our main site, the local private hospital for all cancer ( since early May) and opening a new site in the north of the county some 100 miles of small roads from the centre.
acute trust
For many trusts, there is a challenge in defining 'normal service', and some question whether the pre-COVID level of service is a desirable comparison given many were struggling to meet demand at the time.
Arguably we were not meeting the needs of all patients before COVID-19, and unless the vaccine becomes available it could be a couple of years before we can return to what we were doing before COVID19, although arguably we wouldn't want to simply return to that position.
combined acute and community trust
It is clear that there are different categories of "restoration" - there is that which is straightforwardly about replacing services in the same format with added COVID-19 safeguards, and on the other hand services where experience or strategies/discussions pre-COVID have demonstrated that services should be provided in a different way and they need more work to set up in new sustainable format.
acute trust
Mental health services faced a massive treatment gap prior to COVID-19 - the Five year forward view target for CAMHS was 35% coverage. COVID demand, especially young people, is on top of that. The workforce is already extreme stressed from overwork. This will make that worse.
combined mental health/learning disability and community trust
Overall, trusts are clear that they are committed to returning to a sustainable level of services which meets the needs of as many patients as possible, but emphasise that this may look different to before the coronavirus outbreak, and will rely on continued innovation and sustaining the new ways of working implemented to cope with the outbreak.
The geography of the site makes it more challenging for doubled up services whilst keeping people separate with COVID-19/ suspected COVID-19/ non-COVID needs. New ways of working have meant some waiting lists have improved, others have grown. More planned operations are becoming more urgent. We have already seen people who have left it for too long before seeking help and are too far progressed in their illness to aid recovery, which is heart breaking.
combined acute and community trust