Addressing health inequalities experienced by children and young people requires a holistic approach from a range of public services and government departments, including (but not limited to) education, housing, transport and the criminal justice system. However, trusts can, and do, play a pivotal role as anchor institutions in their communities, by working in collaboration across their health and care systems to invest in more preventative initiatives, and in making every contact count with patients.
Overcoming the barriers
Trusts are facing an unprecedented level of demand on services in the face of backlog recovery from the Covid-19 pandemic. Waiting lists are continuing to rise and services continue to struggle with industrial action. These operational pressures can constrain the capacity for trusts to prioritise efforts to reduce health inequalities. Our United against health inequalities survey of 254 trust leaders in 2021 revealed a huge appetite from trust leaders for tackling health inequalities but identified wider pressures on the system as the main barrier to progress. A key aim of our Health Inequalities programme is therefore to work with trust leaders to embed health inequalities as part of core business, taking an equity lens to addressing operational issues where possible.
This report highlights the importance of trusts recognising the unique experiences of children and young people in their work to address health inequalities. Many health service initiatives are set up with the intention of applying to all ages or are targeted to older populations where acuity may be highest. Arguably, more attention and resource should be targeted at children and young people's services, which can prevent health inequalities from becoming embedded at an earlier stage.
Analysis of local data including local authority Joint Strategic Needs Assessments (JSNAs) and healthcare data from the trust and integrated care system (ICS), is a valuable means of assessing existing inequalities. The Office for Health Improvement and Disparities' child and maternal health data tool provides local authority data on key child health topics, available by deprivation and by regional and national comparisons. Our briefing paper on effective data and insight discusses some of the current challenges around data collection and reporting, that can limit understanding around inequalities in healthcare access and outcomes. Gaps need to be addressed in the recording of deprivation, ethnicity and age. More work also needs to be done to improve data collection processes, to ensure the interoperability of data sharing and embed data reporting in board discussions.
Alongside data collection, trusts can engage with children and young people directly to hear their views and experiences on how their services could be improved. Often young people report negative experiences of healthcare settings, which can be daunting and intimidating. The Office for Health Improvement and Disparities have developed standards for establishing youth friendly healthcare services. In addition, the NHS Long Term Plan sets out a move towards providing zero to 25 years services to improve continuity of care for young people and limit the negative experiences young people often face when they transition from paediatric to adult services at early ages. This reflects a broader shift within trusts to provide person-centred care that meets the individual's needs.
Implementing Core20PLUS5
Core20PLUS5 is NHS England's (NHSE) framework for reducing health inequalities, intended to guide and inform the work of trusts and the wider healthcare system. The approach prioritises attention on five clinical areas where inequalities are particularly pronounced. It directs attention to focusing on the most deprived 20% of local populations alongside the needs of 'PLUS' population groups that require targeted support. The latter are defined locally based on need but could include ethnic minority communities, those with long-term health conditions, groups with protected characteristics or those experiencing social exclusion (also referred to as 'inclusion health' groups).
There are two separate versions of Core20PLUS5 – one for adults and the other for children and young people, developed in collaboration with young people on the NHS Youth Forum. For children and young people, the five clinical areas identified are:
- Asthma.
- Diabetes.
- Epilepsy.
- Oral health.
- Mental health.
There is clear evidence for targeting interventions around these clinical areas, where inequalities are particularly stark. For example, children and young people from ethnic minorities are more likely to be hospitalised with their asthma and those with type 1 diabetes are more likely to have higher haemoglobin subunit alpha 1 (HbA1) rates and are less likely to use diabetes technologies to monitor their conditions, in comparison to white children. Tooth decay is the number one reason children are admitted to hospital in the UK, with concerns that children aged five living in the most deprived areas are three times more likely to experience dental caries, in comparison to those in the least deprived areas. Data also indicate that emergency admissions for epilepsy are higher for children living in the most deprived areas. The mental health and wellbeing of children and young people is a huge public health concern, which has been heightened in light of the Covid-19 pandemic. Adverse childhood experiences contribute to poorer mental health outcomes later in life - with children from the poorest 20% of households in the UK being four times more likely to develop a mental health condition compared to the wealthiest households.
NHSE has set out specific aims for each of these clinical areas. These actions build upon earlier commitments within the NHS Long Term Plan around improving health outcomes for children and young people.
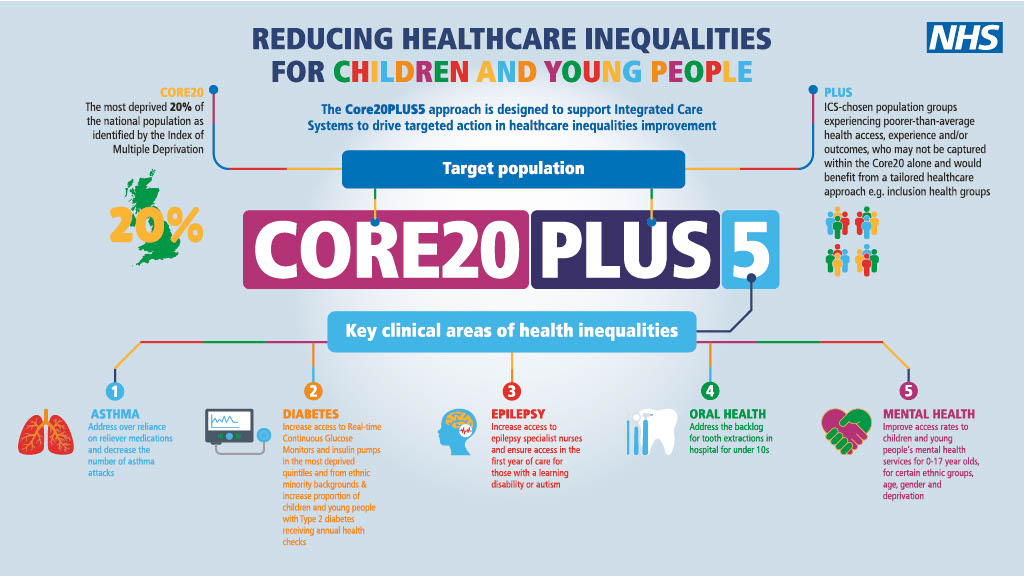
Core20PLUS5 infographic - children and young people