Perceptions of regulation
In the past 12 months operational pressures in the NHS have intensified. The pressures have affected all sectors, with backlogs of care, high levels of demand in urgent and emergency care, significant issues with discharge, and ambulance handover delays, compounded by staff shortages and burnout. However, while the operational challenge has intensified, our survey demonstrates that trusts feel increasingly less confident that regulators understand the pressures they are facing, or are factoring this context into their approach to regulation
and oversight.
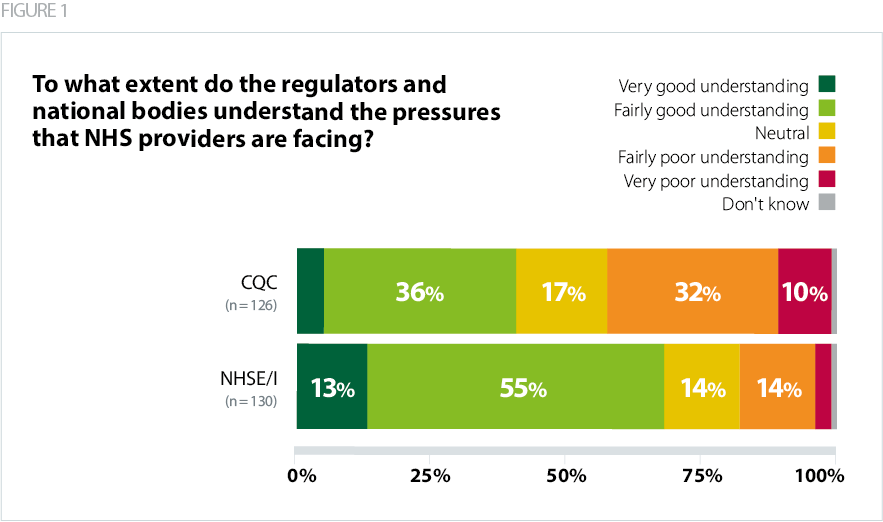
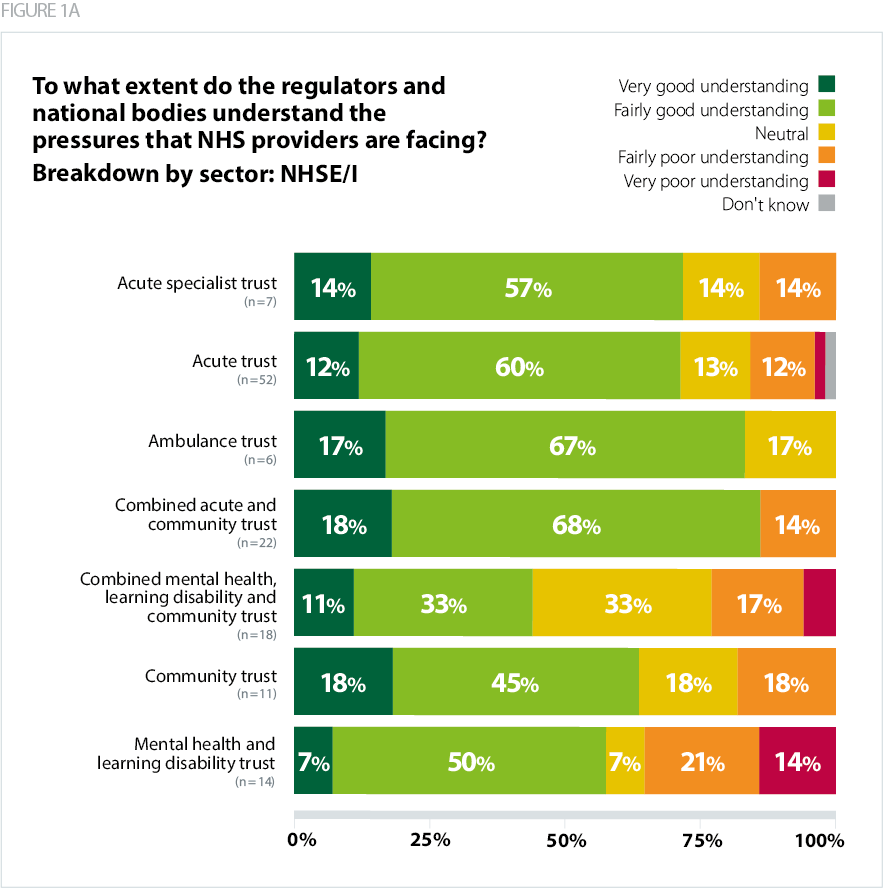
NHS England and NHS Improvement
Just over two thirds (68%) of respondents said NHSE/I had a good (very good or fairly good) understanding of the pressures NHS providers are facing. This compared with 74% in 2019, and 75% in 2018. Those who thought the regulator's understanding was poor (very poor or fairly poor) have increased to 17% this year, as compared with 14% in 2019, and 12% in 2018 (please note this question was changed slightly in the 2020 survey to reflect views before and during the pandemic so is not directly comparable to other years).
It is worth noting that responses varied by trust type. Ambulance trusts (84%) and combined acute and community trusts (86%) were most likely to feel that NHSE/I had a very good or fairly good understanding of the pressures. That compared with only 57% of mental health/learning disability trusts who felt the same way, and 35% rating its understanding as poor.
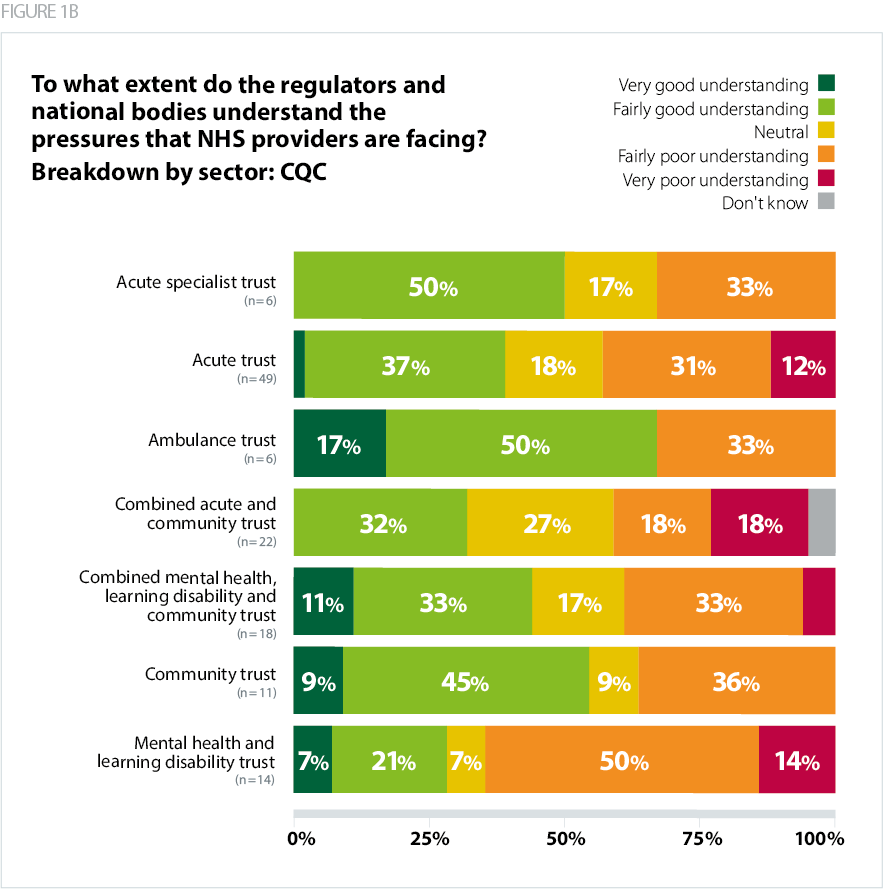
Care Quality Commission
There was an even greater shift in perceptions relating to CQC, with 41% rating CQC's understanding of provider pressures as good. This marks a dip of around 10 percentage points compared with 2019, when 52% described CQC's understanding as good, and a dip of further 10 percentage points compared with 2018, when positive perceptions of CQC's understanding stood at 62%.
Responses again varied by trust type, with ambulance trusts having the highest proportion of respondents who thought CQC had a good understanding of the pressures that NHS providers are facing (67%), followed by community trusts (54%). Mental health/learning disability trusts had the highest proportion of respondents who thought CQC had a very poor or fairly poor understanding of the pressures faced by NHS providers (64%), followed by acute trusts (43%).
Regulatory burden
In similar vein, we have seen deterioration in trusts' perceptions about the burden that regulation places on them. We asked providers whether they thought the regulatory burden and the number of ad hoc requests from regulators had increased, decreased, or stayed the same during the past 12 months. These findings measures the perceived combined burden of regulation from CQC and NHSE/I.
- Just under two thirds (63%) of trusts felt that the regulatory burden had increased over the last 12 months, and only 7% felt it had decreased. In 2020 providers experienced significantly less regulatory activity than in previous years due to the pandemic. Some of the increase may therefore be a result of regulatory activity returning to a more normal pattern. However, if we compare these results with the period before the pandemic, we can see that in 2019, 38% felt the burden had increased and 16% felt it had decreased.
- Perceptions of burden varied by sector. These ranged from a high of 88% among acute specialist trusts who felt the regulatory burden had increased, to a low of 45% among community trusts.
- A reported increase in the number of ad hoc requests from regulators tells a similar story. In total 61% of trusts said these have increased in the past 12 months, while 6% said they had decreased. This compares with 45% and 8%, respectively, in 2019.
- Responses varied again by trust type. The highest proportion of respondents who thought ad hoc requests had increased were from combined acute and community trusts (83%), followed by acute specialist trusts (75%). Respondents from mental health/learning disability trusts were the least likely to think ad hoc requests had increased (36%) and had the highest proportion who felt they had decreased (21%).
Trust representatives have consistently commented on the increasing burden of regulation, and the confusion of responsibility and reporting lines in the new system architecture. Beyond the increasing burden, trust leaders also raised concerns about the approach taken by NHSE/I, relating both to behaviours and increasingly complex lines of reporting.
Comments were also made on the lack of clarity and focus in regulation, as well as a perceived emphasis on auditing and control, ahead of driving improvement. There was a feeling that the acute sector was much better understood than the mental health or community sectors.
Trusts expressed specific concerns about multiple and duplicative requests from regulators, and their unrealistic expectations. These stemmed from insufficient alignment between regulators, and added to the regulatory burden.
In their comments to the survey, and in conversations we have held with them over the past year, trust leaders describe a disconnect between the approach and messaging from regulators at a national level, as opposed to locally or regionally. For example, there were comments around NHSE/I's regional teams being more understanding and supportive of challenges trusts experience than its national team. Conversely, there was support for CQC's national-level narrative around consistent, risk-based regulation, but trust leaders contrast that with the approach taken by CQC's local inspection teams.
A common theme in members' comments was the feeling that regulators have not been sympathetic enough to the COVID-19 situation and the ongoing pressures the provider sector is facing. For example, some commented that CQC inspectors were not willing to listen to staff sharing their concerns about workforce pressures and delayed transfers of care related to the pandemic, which were having a serious impact on services. They felt that the context had not been sufficiently reflected in CQC's inspection judgements.
There needs to be more recognition of the context we are operating in. Not a dilution of standards, but the reasons as to why these may not be being achieved need to be better understood and reflected in any inspection/reports.
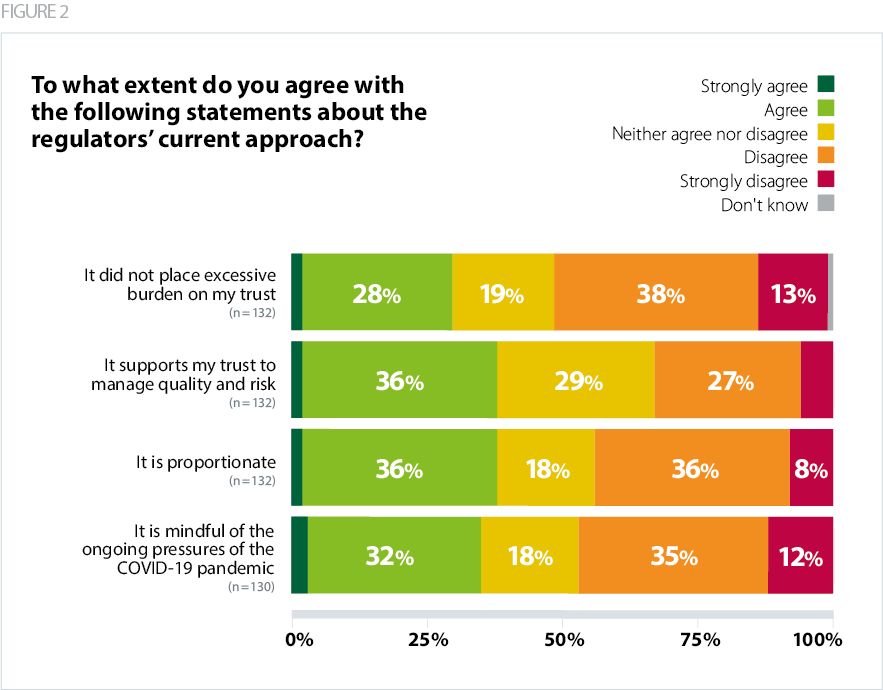
The themes discussed above are clearly reflected in Figure 2, which explores specific statements about regulators' current approach.
- Over half of respondents (51%) felt that regulation placed an excessive burden on their trust. This, however, varied by trust type. While 58% of acute trusts and 57% of mental health/learning disability trusts felt that regulation placed an excessive burden on their trust, only 17% of ambulance trusts and 27% of community trusts felt that was the case.
- More respondents disagreed (47%) than agreed (35%) that regulators were mindful of the ongoing pressures of the COVID-19 pandemic. These perceptions varied again between sectors: 83% of ambulance trusts thought regulators were mindful of COVID-19 pressures, compared with only 14% of mental health/learning disability trusts.
- Similarly, 44% of respondents felt that regulators' approach was not proportionate while 38% said it was. Mirroring the findings on COVID-19 pressures, ambulance trusts were most likely to say the regulators' approach was proportionate, while mental health/learning disability trusts were least likely.
- Views were more positive with regard to regulators supporting trusts to manage quality and risk – 38% agreed that this was the case, compared with 33% who disagreed. There were differences between sectors here too, consistent with findings reported above: 67% of ambulance trusts and 63% of acute specialist trusts felt they were supported to manage quality and risk, while only 14% of mental health/learning disability agreed with this.
I understand the need for information and regulation, but it's growing disproportionately to any benefits this brings.