

Week seven of the winter sitreps shows that despite another week of high demand, overall trusts continue to cope well, partly aided by a less severe flu season and milder weather. However we remain concerned that performance could suffer if deteriorating weather and conditions for norovirus and flu lead to a spike in demand in the coming weeks.
Key indicators this week reflect trusts’ resilience in the face of rising demand:
- bed occupancy remains high at 94.6%, a slight drop of 0.1% from last week, and similar to the level at the same time last year (94.8%).
- escalation beds increased by 91 to 3,703, a new high for this winter but still considerably lower than the same point last year.
- total beds open also reached the highest level of the winter so far (97,580), but this is 643 fewer than the same point last year.
- long-stay patients are holding steady. Those staying over 7 days increased by 0.4% since last week, but there were 1.3% fewer patients staying over 14 days, and 2.2% fewer staying over 21 days compared to last week.
- beds closed with D&V and norovirus fell by 8.1% since last week to 567. This is 175 fewer than the same point last year.
- there were 35 A&E diverts this week, down from 38 last week.
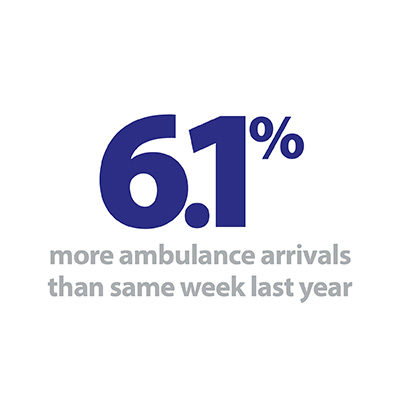
- ambulance arrivals fell again slightly by 1.2% this week to 97,577, but remain much higher than the same point last year.
- the proportion of ambulance arrivals waiting more than 30 minutes dropped by 0.8% to 11.7%, while those waiting more than 60 minutes also fell by 0.4% since last week to 2.4%.
Trusts have directed substantial efforts towards appropriate discharge and greater support for patients once they are outside the hospital setting, to improve recovery and reduce risks of readmission. The numbers of long stay patients have remained well below the levels seen last winter, giving some degree of confidence that hospitals will be better placed to cope with demand increases as and when they occur.
In our guest blog this week we hear from Nicola Plumb, director of organisational development, participation and corporate Affairs at Dorset Healthcare University NHS Foundation Trust, and James Donald, head of Communications at Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust, who outline the benefits of system working to provide the best care in the best place for the local population.
A large part of their success is a result of reducing hospital admissions, both through an effective triage service in emergency departments and via greater integration with community services to help patients manage their conditions. Strong uptake of digital technology has also played a part in driving a collaborative approach, meaning patients can access support from a range of providers without physical barriers of transport and infrastructure limiting availability.
Positive developments such as these are necessary to enable trusts to keep pace with demand for services which remains extremely high. Acute bed occupancy alone points to a system stretched to its limits, and with ambulance arrivals this week higher than all but one week last winter, trusts will feel there is little wriggle room operationally. While performance so far this winter has been markedly better than last winter, trusts still face significant challenges to maintain this. We should not overlook the sustained dedication of staff who are working so hard in all corners of the health and care landscape to keep services running this winter.
For a more detailed breakdown of this week’s winter sitrep data please see our summary dashboard.
Best care in the best place in Dorset
In Dorset planning and partnership working is king and it is not something that is just the domain of winter. The Royal Bournemouth and Christchurch Hospitals (RBCH) and Dorset Healthcare University NHS Foundation Trusts have very successfully been collaborating as part of a move towards complete system working under the banner of Our Dorset.
Both trusts have a number of initiatives and teams in place to ensure that their patients are getting the best care, in the best place. Cherry McCubbin is RBCH’s associate director for older people and integrated care who works closely with colleagues in her trust and also out in the community to ensure that patients are discharged when they are medically fit and that ongoing support is given to make sure they are not readmitted to hospital. This involves physiotherapists and occupational therapists going out to provide follow up care at home and teams from the community trust – Dorset Healthcare – providing ongoing support and care.

The Royal Bournemouth and Christchurch Hospitals and Dorset Healthcare University NHS Foundation Trusts have very successfully been collaborating as part of a move towards complete system working under the banner of Our Dorset.
The RBCH has also recently brought one of the community wards onsite and Fayrewood ward now provides rehabilitation for patients who are medically fit and need some extra support to ensure they are ready to go home. Having the ward onsite means patients can be easily transferred from an acute or specialty ward and if for any reason they deteriorate they can benefit from still being in an acute hospital.
But preventing patients being admitted to hospital in the first place is a priority and last year RBCH introduced triage staff to its emergency department. Senior clinicians are able to quickly see and assess people coming to ED and in many cases redirect them to the urgent treatment centre onsite or back to their GP, NHS 111 or pharmacist. In addition to this, Dorset Healthcare now has more staff onsite at RBCH to help the trust manage the complexity of patients coming to ED and being admitted. Emma Williams, head of integrated services for East Dorset, describes how they are doing this and what they doing to help patients manage their conditions and be cared for in the right place
"Over the last 10 weeks we have had community matrons and an intermediate care therapist based in the emergency department at the Royal Bournemouth to help manage the patients coming in who can be cared for by our integrated hub in Bournemouth or co-located teams in Christchurch where there is access to both health and social care services. In many cases we know these patients already and can help them to avoid an unwanted admission to hospital."
Our district nurses are now attending the stranded patients meetings and looking at patients with seven day stays and helping to arrange what is needed in order for them to be discharged.
Head of integrated services, East Dorset
"Our teams are also building relationships with the wards and raising awareness of what help we can give and sharing our knowledge of the patients that we already support in the community. Our district nurses are now attending the stranded patients meetings and looking at patients with seven day stays and helping to arrange what is needed in order for them to be discharged. Initially we focused on the patients who had been in for 21 days or longer but by that point they could be deconditioning and are at a much higher risk of infection.
"This all means that we have excellent links into the Royal Bournemouth and are working closely across the whole hospital.
"We also proactively track our patients who have been admitted for between three and seven days to Poole hospital and create an inpatient list on our virtual ward and this also includes patients with a planned admission. This means we can plan for their discharge before they become at risk of infection and de-conditioning and make sure the health and social care teams are ready to take over their care."
Through integrated community and primary care services, GPs are able to discuss patients with clinicians and work through current issues and provide some enhanced community support if needed.
This proactive approach to caring for patients and working in partnership is clearly starting to pay dividends so that between 21 December and Christmas Eve, the Royal Bournemouth was able to discharge 100 more patients compared to in 2017 and ensure that those patients were home for Christmas.
Dorset has made some very positive progress towards preventing admissions and through the use of digital technology, including tele-health and teleconferencing, they are able to help nursing and care homes avoid calling for an ambulance in some instances and the resident ending up being admitted to hospital. Through integrated community and primary care services, GPs are able to discuss patients with clinicians and work through current issues and provide some enhanced community support if needed.
Emma Williams add: "Collaborating together and getting over the boundaries of who provides what means that the patient is at the centre of all we do. We can keep the flow going through all services by working together and making sure that patients are receiving the right care in the right place and where possible that is at home where patients want to be."
Trusts working extremely hard to maintain performance as winter takes hold
Responding to the latest set of weekly winter performance data, NHS Providers director of policy and strategy Miriam Deakin said:
"Winter is starting to take hold, but trusts and NHS staff are working extremely hard to maintain current performance for patients.
"The number of beds in use remains high but is at a similar level to the same point last winter. Trusts have had to open more beds to meet this demand but fewer than at the same point last year.
Winter is starting to take hold, but trusts and NHS staff are working extremely hard to maintain current performance for patients.
Co-Director of Development and Engagement
"Efforts to get patients out of hospital and with care closer to home are paying off. This is down to more joined-up working with partners across health and care service.
"It is good to see a fall in the number of delays of patients handed over from ambulances to hospital. Yet, ambulance services continue to experience very high demand this winter.
"NHS trusts will remain vigilant and prepared as colder weather sets in. The public can also help alleviate pressures on A&E by seeking advice from 111 when they don’t require emergency care."