
The latest week of the winter sitreps sees continued resilience against rising demand as we approach the mid-point of winter. Improvements to patient flow have led to better performance so far compared with last year, but with cold weather on the way services will be severely stretched if demand keeps increasing.
Key indicators this week:
- Bed occupancy is now at 94.7%, up a further 1.5% in the past week and very similar to the same point last year.
- The number of escalation beds open increased by 18% in the past week to 3,612, the highest of the winter so far, but still 22% lower than the level seen in the same week last year.
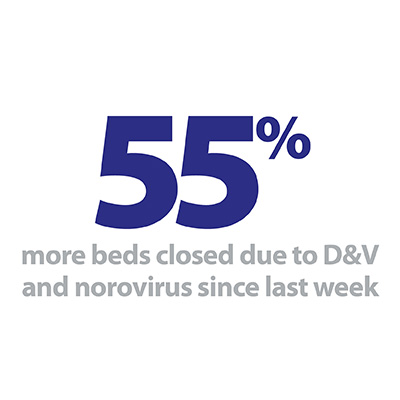
- D&V and norovirus are increasing in hospitals with 617 beds closed this week, a rise of 55% on the previous week.
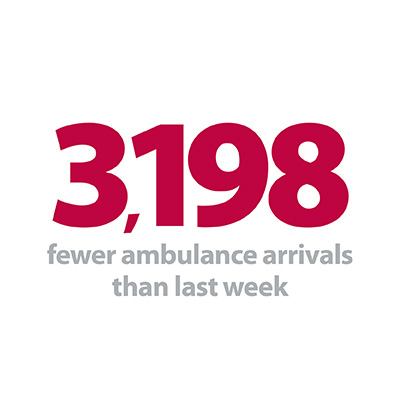
- Ambulance arrivals declined by 3.1% in the past week, but are still extremely high with 14,107 arrivals per day and still much higher than the same week last year.
- Handover delays rose for the fourth consecutive week, with 1 in 9 ambulance arrivals now waiting half an hour or more.
- Long stay patient numbers continue to rise: those staying over 7 days increased by 1.2% in the past week and there were an additional 445 patients staying longer than 21 days, 2.9% more than last week.
- A&E diverts more than doubled in the past week to 38.
Despite high bed occupancy, trusts have not yet opened the number of extra beds that they did last year. While both handover delays and length of stay are rising, they remain in a better place this winter, leading to hospitals being able to use beds and resources more efficiently. This has a positive impact on both staff and patients who are able to return home or other care settings when appropriate.
While both handover delays and length of stay are rising, they remain in a better place this winter, leading to hospitals being able to use beds and resources more efficiently.
Local innovation and planning, such as the techniques described in our guest contribution this week from Simon Barton, Chief Operating Officer at Sherwood Forest Hospitals NHS Foundation Trust, demonstrate the practical steps trusts are taking to meet the winter challenges. These include converting wards and encouraging flexibility of teams in anticipation of demand, funding private beds in the community, as well as maintaining a positive staff culture that values agility and adaptation to deliver benefits to patients.
Again we are hearing from trusts that people arriving at hospital are sicker and require more complex care the further we get into winter. This continues to place an ever increasing importance on the ability of the system to work efficiently to stay afloat. Trusts have performed admirably to reach this point, but will be hoping that conditions do not deteriorate in coming weeks so current levels of care can be maintained.
For a more detailed breakdown of this week’s winter sitrep data please see our summary dashboard.
In our trust perspective this week, Simon Barton, chief operating officer at Sherwood Forest Hospitals NHS Foundation trust, writes on how their trust prepared for the winter period.
Preparing, enacting and reacting
Preparing
There were a number of lessons in how we planned and rolled out our 2017/18 winter plan.
We used a new process involving collecting more ideas from divisions, followed by table top exercises with staff to test scenarios. This allowed us to see what was realistic (both in terms of staff and cost, acknowledging that we weren’t going to be able to recruit lots of new staff), what was within our ability to change and what we might need to work with partners on.
We used this to form the basis of the winter plan which was taken to and signed off by our Board in August 2018, giving us plenty of time to communicate it out to staff and ensure the changes and increases to beds happened when we told SFH colleagues they would.
The overarching aim was to ensure there was sufficient capacity to meet demand, maintain patient safety and patient flow throughout the winter period.
Chief operating officer, Sherwood Forest Hospitals NHS Foundation Trust
The overarching aim was to ensure there was sufficient capacity to meet demand, maintain patient safety and patient flow throughout the winter period. The key principles for the winter capacity plan were:
- To have a maximum length of stay of 19 hours on the Emergency Assessment Unit (EAU).
- To achieve a 92% bed occupancy rate on base wards.
- To create additional capacity, equivalent to one ward, over and above the capacity available during winter 2017/18.
Enacting
To do this we opened an additional 35 beds compared to winter 2017/18, by converting a surgical ward to a medical ward for two months, opening extra medical beds and funding an extra 20 beds with a private provider in the community. We also looked at our activity and planned day case procedures in periods we know would be busy to reduce demand on inpatient beds.
One of the key enablers has been the flexibility of the teams at SFH to working differently over the winter months, for example surgical colleagues agreeing to be part of the medical ward teams. We are fortunate with our culture at SFH that our colleagues are always prepared to try new ways of working if they can see what the hoped benefits to patients will be. We had trialed this last winter and it had worked well so it was one of the areas we wanted to see if we could build on for this year.
We are fortunate with our culture at SFH that our colleagues are always prepared to try new ways of working if they can see what the hoped benefits to patients will be.
Chief operating officer, Sherwood forest hospitals NHS Foundation trust
We rolled out our plan on agreed dates with our staff ensuring that changes were planned and delivered on that date and not all the capacity was changed or opened at once, meaning it was incrementally opened over a seven week period.
Reacting
Once our capacity is in place we react to fluctuations in demand by using our escalation actions, an agreed set of actions that help us maintain patient access and ensure safety by reducing exit block from the ED.
As well as the usual communications tied in with the national Help Us Help You campaign, we also put out additional messages around flu, norovirus and using services wisely ahead of specific dates where we would anticipate increased patient activity e.g. the Friday before Christmas, Boxing Day, the first Monday after Christmas and New Year’s Eve.
Results
Based on our plan we were expecting our four-hour performance to be around 90.5% so it is testament to the hard work of the teams across SFH that for December we were at 94.9% (and year to date we are still above 95%). While not meeting the target, it was an improvement on our performance in December 2017 (86.4%) and the variation in performance in month compared to last year has improved from a 20% range to a 10%. Our admissions have been high, 86 per day via our ED in December 2018 compared to 83 per day in December 2017. However, length of stay has been lower which has enabled us to cope better. The anecdotal feedback we’re getting from staff is that they feel the roll out was much smoother this year and has felt calmer across our sites so far. We feel we are working better with partner organisations which is evidenced in ambulance handovers performing better than last year and improved discharges. All this means a better experience for some of the sickest patients we see.
Our response: Winter is making an impact but trusts are coping
Responding to the latest weekly winter performance data from NHS England, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"The figures this week show that the winter is making an impact, but trusts are coping, with staff working tirelessly for their patients.
"Falling temperatures and rising cases of flu and norovirus are adding to already exceptionally high demand for NHS emergency care. Bed occupancy has risen to 94.7% from last week, and trusts are telling us that people arriving at hospital are sicker, requiring more complex care.
Falling temperatures and rising cases of flu and norovirus are adding to already exceptionally high demand for NHS emergency care.
Co-Director of Development and Engagement
"Despite high bed occupancy, trusts have not yet opened the number of extra beds that they did last year. The efforts to reduce the number of patients staying over 21 days mean beds can be used more efficiently, allowing patients to return home or into community care when appropriate.
"The demand for ambulance services remains exceptionally high, with around 14,100 arrivals at hospital each day. As a result of the pressures inside and outside hospitals, delays in handing over patients to A&E departments are beginning to grow. This is a clear indicator that winter pressure is mounting throughout the health and care system."