The underfunding and failure to allocate limited resource to where it is most needed are well established problems that are being keenly felt on the frontline. However, it is possible to imagine major improvements being made to services under a more appropriate capital system.
This section describes the opportunity that investing more in infrastructure presents, spanning the patient experience, and a number of themes highlighted in the long term plan – expanding diagnostics capacity, transforming care pathways, and creating a fully digitised, technologically enabled service.
The patient experience
Trusts need to invest in services in order to keep up with rising levels of need, deliver improvements in the quality of patient care, and meet rising public expectations about the way they interact with services.
Reducing delays due to equipment failure
Trusts need resilient infrastructure to guarantee the smooth running of services. For example, at University Hospital Southampton NHS Foundation Trust, a high voltage power failure led to the closure of almost all clinical services for eight hours. This led to 1,788 cancelled outpatient appointments and 99 cancelled elective procedures (although all were subsequently rescheduled).
Other trusts have described problems with ventilation machinery, which can put theatres out of action for several days. Plant equipment also needs to be well maintained to ensure clinical functions run smoothly, for example the supply of medical gas. Access to appropriate capital funding could lead to a wholesale upgrade of supporting infrastructure, limiting cancellations and helping ensure patients are treated on time.
Investing in improved diagnostics equipment, such as MRI and CT scanners, X-ray machines and ultrasound equipment, will speed up diagnosis and identify diseases and conditions much more quickly. Early diagnosis, particularly in cancer, can save lives and avert treatment costs. Improving diagnostic capacity is a key ambition of the long term plan and is discussed in more detail below.
Increasing ward capacity
During summer 2019, NHS England chief executive Simon Stevens warned the existing bed stock in the NHS was "overly pressurised" and said the NHS would need more bed capacity to deal with demand. There is a strong correlation between the NHS being unable to meet the four-hour accident and emergency target and high occupancy levels: bed occupancy above 88% across the NHS as a whole is a strong predictor of the service being unable to maintain performance within the standard.
Since quarter two 2010/11, the NHS has been unable to meet the four-hour target and occupancy levels have consistently exceeded 90%. Without significant capital investment to increase the bed base by around ten percent, patients will continue to wait longer to receive treatment.
Investing in new ward capacity also has the potential to reduce staffing costs: trusts tell us that using overspill space or side rooms to add capacity requires more intensive use of staff to guarantee safety than a modern, properly designed acute ward. Where trusts become reliant on using additional beds, their staffing costs can rise disproportionately.
There could also be a positive impact on staff wellbeing. One trust explained how rooms designed for staff were being used to treat patients, which meant there were no suitable rest areas for staff on breaks between busy shifts. Trust environments should ensure staff safety and remain conducive to relieving stress. If the NHS cannot provide good working environments for staff, this will have a negative effect on patients.
Improving safety and quality
Some trusts need more capital funding to deliver programmes that reduce safety risks and improve the quality of care. The mental health sector's estate was described in DHSC's independent review of the Mental Health Act as "the worst estate that the NHS has". For many providers the priority will be to remove fixed ligature points – currently 75% of people who die from suicide while on a psychiatric ward do so by hanging or strangulation. For some mental health providers there is a similarly urgent need to remediate accessible flat roofs which can lead to patient harm.
In the acute sector, there are emergency departments where staff cannot maintain clear lines of sight to more unwell patients. Some trusts have installed nurse alarms in high-risk areas on wards as a workaround. Kettering General Hospital NHS Trust has an ambition to open a dedicated paediatric entrance waiting treatment and observation area to make it easier for staff to observe patients.
Improving patient flow
Patient flow could be dramatically improved through increased access to capital funding. Too often, hospital layouts do not support modern healthcare.
Many trusts wish to redesign and relocate their emergency departments to establish a better integrated service. For example, Hampshire Hospitals Foundation Trust plans to relocate its orthopaedic outpatients department so it is adjacent to its emergency department. This approach will enable multi-disciplinary working which is focused on rapid triage and assessment, and will stop patients being bounced around multiple sites. Widespread improvements of this kind could be delivered with an increased and properly-allocated capital budget.
The long term plan recommends creating “hot” and “cold” sites which separate planned services from urgent and complex services. It is hoped this model will improve performance of urgent and emergency care, including the speed of ambulance handovers.
The long term plan recommends creating "hot" and "cold" sites which separate planned services from urgent and complex services. It is hoped this model will improve performance of urgent and emergency care, including the speed of ambulance handovers. The plan suggests NHS England and Improvement will back providers wishing to pursue this model, but in reality this will require extensive capital funding.
In addition to these improvements, trusts can also invest in more advanced programmes to help improve planning, scheduling and flow. Patient flow technology, such as radiofrequency identification and the use of control centres, can reduce length of stay, improve A&E performance and increase available capacity. Some trusts have already been able to make this investment, such as the Royal Wolverhampton NHS Trust. As a result, the turnaround of vacant beds has been significantly improved.
However, improving patient flow may not always require services to be rebuilt: it may be as simple as reducing the reliance on faulty lifts. In one trust, lift repair works can make transferring patients from one building to another impossible without an ambulance. This leads to delay and a waste of money.
Improving patient experience
Reducing waiting times and improving safety, quality and flow all improve the overall patient and service user experience and will support better outcomes. However, there are other opportunities to materially improve the way patients receive care, from properly insulating wards to designing environments that make more use of natural light. Temperature control is a problem for many trusts with ageing buildings, with some wards exceeding 30 degrees during the summer. We also heard from a community provider which had to buy electric heaters and put tape around its single glazed windows during cold winter weather.
Mental health trusts would like to invest in the removal of the 350 dormitory wards that still exist in the NHS. In December 2018 the independent review of the Mental Health Act made a number of recommendations to the mental health estate:
Poorly designed and maintained buildings obstruct recovery by making it difficult to engage in basic therapeutic activities (getting outdoors or social interaction with others) and contributing to a sense of containment and control. Wards are experienced as cold and impersonal places, that some say are more similar to a prison than a hospital, making a return to the community, with all its everyday stimuli and risks, more challenging. We are calling for a major capital investment in the NHS mental health estate as part of the proposals from the NHS for a multiyear capital plan to support the long term plan.
There is also evidence to suggest that therapeutic environments are linked to improved rehabilitation in mental health services.
Delivering the long term plan
The long term plan sets out how the NHS needs to adapt over the next ten years. It details new service models, action on prevention, progress on care outcomes, the NHS workforce, digitally enabled care, and improving value for money. But the plan is clear that upfront capital investment will be needed to deliver on those recommendations.
Diagnostics
The long term plan calls for a wholesale upgrade to existing diagnostics infrastructure. It explicitly states that a capital settlement is needed to invest in new CT and MRI scanners to deliver faster and safer test results. This is to support the ambition for the proportion of stage 1 and 2 cancer diagnoses to rise from around 50% to 75% of cancer patients by 2028. It will also help the service deliver on a new faster diagnosis standard for cancer to be rolled out so patients receive a definitive diagnosis within 28 days.
The UK already lags behind peers on the number of CT scanners in operation. But much of the existing stock is faulty and unreliable. For example, at University Hospitals of Morecambe Bay NHS Foundation Trust, between June and July 2019 two CT scanners developed faults at the same time, resulting in reduced activity for 270 hours over a twelve-day period, affecting over 500 scheduled CT scanning slots.
Digitally enabled care
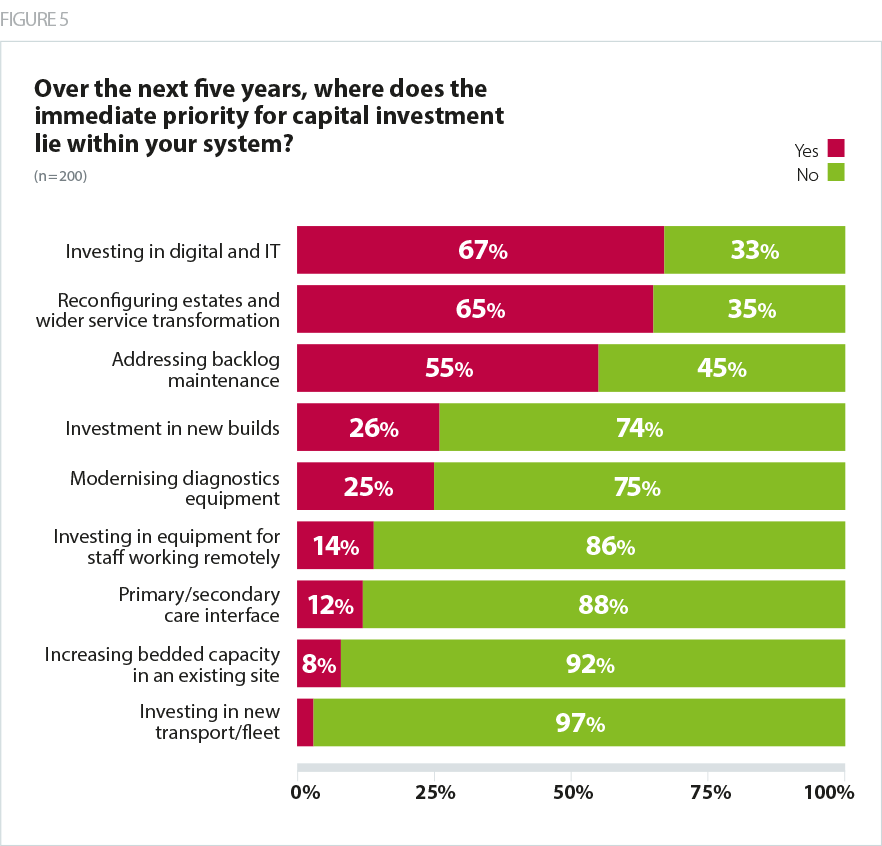
Our survey results revealed the most commonly cited capital priority/opportunity was investment in digital and IT (67%), followed by general reconfiguration of estates and wider service transformation (66%) and addressing the backlog maintenance (55%).
The long-term plan commits to the NHS to be 'digital first' within ten years. Particular attention is given to digitally-enabled primary and outpatient care.
There is a commitment to shift towards models of outpatient care that do not rely on face to-face consultations, with the aspiration that around 30 million hospital visits a year can be avoided. Where capital has been available, trusts have already begun implementing digital alternatives. At University Hospitals of Morecambe Bay NHS Foundation Trust, the trust has already rolled out digital services for the Cumbrian town of Millom, which is saving patients and staff mileage and time. Other trusts are already looking at how they can better manage their estate as they move towards digital outpatient services, for example potentially building on car parking space as the number of visits is reduced.
It is also well known that improved IT capacity can help maximise the value of clinical time, but this again requires investment in digital infrastructure. For example, one trust in the south east has set up a virtual fracture clinic, enabling patients to be assessed ahead of their appointments. This has led to the cancellation of more than three quarters of new patient appointments in favour of GP-led self management, freeing up consultant time for urgent referrals from elsewhere.
Investing in technology remains important in supporting new remote and flexible working. This is particularly important for trusts which provide healthcare remotely and in the community, as delivering care remotely can reduce the time clinicians spend driving between appointments. Where trusts have implemented electronic patient record systems and smartphones or tablets, staff can access data remotely. This can create flexible working spaces, allowing clinicians to work from different locations, and can also encourage healthier work-life balance if staff are able to work from home. National leaders have noted that failing to invest in technology risks frustrating staff who may choose to leave the NHS for other sectors.
Financial and clinical sustainability
Capital investment will also support trusts to deliver financially and clinically sustainable services. Failing to invest in infrastructure is a false economy. Many investments often deliver significant financial savings, whether through consolidating back office services, or replacing paper with electronic care records. For example, Liverpool Women’s NHS Foundation Trust plans to build a new hospital which would be physically joined to the new Royal Liverpool and Broadgreen University Hospitals NHS Trust by a bridge. This would deliver value for money as co-locating services would enable the organisations to reduce costs by sharing services such as facilities management.
Existing clinical configuration can sometimes be the accident of history rather than design. At University Hospitals of Leicester NHS Trust, for example, the trust’s maternity and neonatal services are spread across two sites. This duplication means staff and equipment are spread too thinly, and the service is expensive to run. Care Quality Commission and NHS England have raised concerns over the safety and quality of the configuration of this service. The trust has now received funding from the government to consolidate this service onto a single site. Quality and clinical outcomes will improve. Similar situations exist across the country.
Transforming ambulance services
In the ambulance sector, a better capital settlement could enable trusts to invest in fleet, reconfigure estate to improve efficiency, and invest in digital transformation to improve resilience and responsiveness.
Ambulance trusts must be able to reach people across wide geographies within minutes, and need to run and maintain many sites. Their estates are therefore complex and varied. They typically include a headquarters and control centres where hundreds of people are based, and dozens of ambulance stations of varying size. However, too often trusts do not have buildings that support the best use of staff time and resources. For example, many smaller ambulance stations are decades old and expensive to heat. In extreme cases stations are not large enough to accommodate modern larger ambulances.
Ambulance trusts must be able to reach people across wide geographies within minutes, and therefore need to run and maintain many sites.
Lord Carter's 2018 review of operational productivity in the sector recommended trusts adopt a "make ready" system, in which ambulances would begin and end their shifts at hub sites where all maintenance work can be carried out, before being deployed to smaller local stations ready to be called out. Lord Carter found this model makes better use of clinical staff time, and reduces running costs by enabling trusts to rationalise their estate. It also facilitates better asset management and infection prevention and control processes. However, to implement it, trusts need the right facilities in the right places across their geography, and may need to spend capital to build new, fully equipped hub stations. Yorkshire Ambulance Service NHS Trust estimated the cost of implementing this model at around £70m.
Ambulance trusts also need to invest more in IT to drive transformation. One major opportunity is for providers to jointly invest in common computer aided dispatch systems, telephony systems and a common triage tool. This would bring two advantages. First, it would give neighbouring trusts visibility of each others’ fleet, which would make it much easier to lend support or capacity to one another when needed. Second, it would bring significant opportunities to improve resilience in the event of a critical IT failure or loss of a control room. However, such systems represent an investment of many millions of pounds which has not been possible for some trusts in recent years.
Ambulance services function at the heart of the urgent and emergency care system, interacting with all other health sectors and social care. It is therefore imperative to invest to build robust and reliable IT infrastructure that can support real-time communication with a mobile, dispersed workforce, as well as being able to share patient information and care plans across interoperable systems.