Recruitment and retention as well as the supply of new staff is a vital factor in understanding and closing the workforce gap.
Provider trusts are employers and have a responsibility to make their organisations great places to work. There is certainly more that trusts can do. At the same time, retention is becoming increasingly difficult given the mounting pressure the sector as a whole is under.
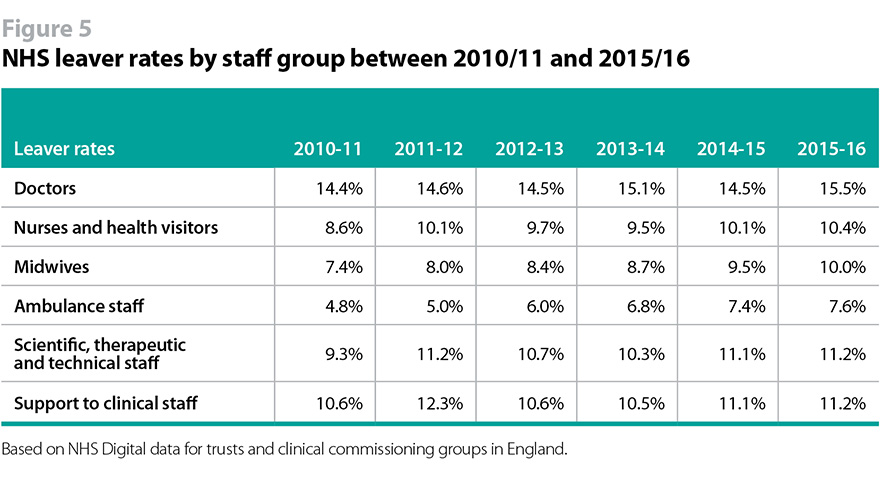
National data shows that across staff groups there is a common trend of rising leaver rates since 2010-11. Figure 5 illustrates the increase for doctors (14.4% to 15.5%), nurses and health visitors (8.6% to 10.4%), midwives (7.4% to 10.0%), ambulance staff (4.8% to 7.6%), support to clinical staff (10.6% to 11.2%), and scientific, therapeutic, and technical staff (9.3% to 11.2%).
The publicly available retention data cannot be broken down by region and importantly does not distinguish between staff who leave one NHS organisation to work in another and those who leave the NHS altogether
What is clear is that there is no point training and recruiting staff to work in the NHS if they then leave and do not return.
The challenge for provider trusts
Provider trusts recognise this and have had a sustained focus on making their organisations great places to work. NHS Employers has a programme to support trusts to improve retention and has recently launched a new toolkit.
Figure 6 illustrates that the proportion of staff who would recommend their organisation as a place to work has actually increased between 2012 and 2016.
Figure 6a
NHS staff survey responses between 2012 and 2016
Figure 6b
Yet there is much more that provider trusts need to do to make their organisations great places to work.
Bullying remains a real concern. 25% of staff reported experiencing harassment, bullying or abuse from fellow staff in the 2016 NHS staff survey, similar to recent years. Black and minority ethnic (BME) staff are more likely to experience harassment, bullying, or abuse. The workforce race equality standard has powerfully shone a light on the experiences and career opportunities of BME staff and trusts must demonstrate progress on developing positive and inclusive cultures and valuing and improving the experiences of BME staff.
There is also a great deal that trusts can do to improve junior doctors’ experience of working and training in the NHS. Following the acrimonious junior doctor contract dispute, many trusts, in addition to implementing the new contract, have begun to make changes to address non-contractual day-to-day issues. NHS Improvement has helpfully collected some case studies.
More widely, there is also a need for a new psychological contract for generations of younger workers who are looking for a different employment relationship, as highlighted by Mind the gap: Exploring the needs of early career nurses and midwives in the workplace, commissioned by NHS organisations in Birmingham and Solihull with Health Education England.
‘Generation Y’ (born 1980-94) make up an increasing proportion of the NHS workforce, as earlier generations reach retirement age or take early retirement. Also known as ‘millennials’, these younger workers tend to be career motivated and want support from their employer to achieve. They value flexibility and work-life balance is a must. They also tend to be prepared to seek work opportunities elsewhere if their needs are not met.
Meanwhile, ’Generation Z’ (born 1995-2012), who are only just beginning to enter the NHS workforce, tend to be less likely to engage with traditional work environments, are likely to move jobs, and are fully immersed in digital technology.
If the NHS wants to recruit and retain younger generations, it will have to adapt its employment offer or they will go elsewhere. The secretary of state recently announced (Conservative Campaign Headquarters) pilots of new apps to improve flexible working for NHS. Greater flexibility is a good starting point. Yet while there is a lot of discussion of working generations within the NHS, it is yet to translate into widespread practical action on the ground, and there is a sense that other sectors of the economy have been quicker to adapt their employment offers.
National-level factors influencing staff experience
There are, however, critical factors that are largely outside of provider trusts’ control. In particular, it has become increasingly difficult to retain staff as the job gets harder, workforce development budgets are cut, and real pay continues to fall.
As one trust leader put it: “The NHS is significantly dependent on the 'heroic' efforts of clinical and non-clinical colleagues in responding to increasing service demand within an environment of ever-challenging financial constraints (including pay/reward controls) that compromises work/life balance, learning and development and overall job satisfaction.”
Figure 7 illustrates that work-life balance is now the fastest growing reason for voluntary resignation of NHS staff.
Figure 7
The growth in work-life balance as a reason for leaving the NHS probably reflects the impact of the discretionary effort staff are being asked to put in. This was shown in the 2016 NHS staff survey, illustrated in figure 6 above, where 59% of staff reported working additional unpaid hours, up from 57% in 2012. It may be reasonable to ask staff to occasionally work extra hours, but to ask them to do so regularly as at present is not sustainable. When asked for some of the biggest challenges to recruitment and retention at their trust, 60% of trust chairs and chief executives cited work pressure.
NHS Employers analysis of its staff retention programme it delivered with provider trusts has found career development and ongoing training were key reasons for staff choosing to stay in or leave their jobs. Yet the workforce development funding (often used for continual professional development) distributed among trusts by Health Education England (HEE) has been cut. In 2015 it was £205m but this year it is £83m (Nursing Times). The cuts reflect reductions to HEE’s own budget, but it has left a funding gap that provider trusts are unable to fill given the pressure on their finances. These cuts to workforce development funding also have an adverse impact on retention and hamper trusts efforts to make their organisatins great places to work for staff who value career development.
Between 2010 and 2017 the real value of NHS staff’s pay has also fallen by 6% (The Health Foundation), while in the economy as a whole it has fallen by only 2% and pay restraint has begun to bite in terms of recruitment and retention. When asked about the biggest challenges to recruitment and retention at their trust, 38% of trust chairs and chief executives cited pay and reward. According to the Institute of Fiscal Studies, the cost of a 2% pay award for the NHS would be £1bn annually (BBC). This level of funding cannot currently be absorbed within the existing financial allocation for the NHS. Therefore an end to pay restraint must be fully funded. Even then, there is a serious risk that ending pay restraint eats up most or all of the extra NHS £8bn promised in the Conservative manifesto. This cannot happen when we have so many other pressing demands. Difficult decisions will need to be made and it is particularly important that such decisions are made with rigour and careful thought. Trusts support the pay review body mechanism as the best way to ensure this.
Provider trusts believe that more could be done at a national level to promote the NHS as a great place to work and make the most of the resonance of the NHS brand across the country. National campaigns have been used for school teachers and the armed forces.
Making the NHS a great place to work – what needs to happen
Provider trusts should:
- continue to prioritise making their organisations great places to work, fostering positive and inclusive cultures, eliminating bullying at all levels, and delivering progress against the workforce race equality standard.
The government should:
- take a realistic view of what is asked of the NHS and the funding they are allocated in order to alleviate the stress and pressure on NHS staff which is contributing to the workforce gap. Staff need to feel that the job is ‘doable’ and that they can care for patients and service users safely. We have previously backed calls for an Office of Health and Social Care Sustainability which could promote a realistic assessment of what is needed;
- set out a plan to deliver the promised end of pay restraint during this parliament. According to the Institute of Fiscal Studies, the cost of a 2% pay award for the NHS would be £1bn annually. This level of funding cannot currently be absorbed within the existing financial allocation for the NHS. Therefore this must be fully funded;
The Department of Health and the NHS national bodies should:
- reverse the cuts to workforce development funds distributed to trusts by HEE, to support staff retention and the delivery of sustainability and transformation partnerships and new care models;
- work with trusts and unions to deliver a national recruitment campaign for the NHS, promoting healthcare careers and the NHS as a great place to work;
- continue to support provider trusts with programmes to reduce leaver rates and improve retention rates.