Today NHS England and NHS Improvement published the final week of the winter sitreps for 2020/21, which marks the end of our Winter Watch campaign this year. The number of COVID-19 patients continues to fall, and there are now fewer than 10,000 patients in hospital for the first time since early November. Pressure is still high in critical care, and while we are starting to see reduced hospital admissions, serious illnesses and deaths in the groups who received an early dose of the vaccine, we know that younger age groups continue to be affected in high numbers.
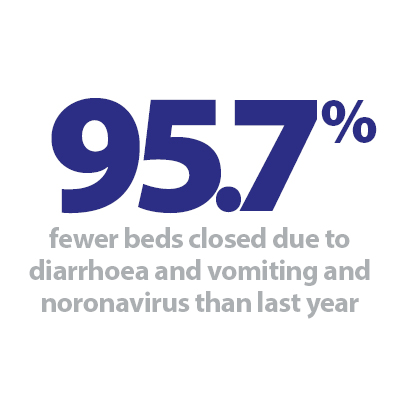
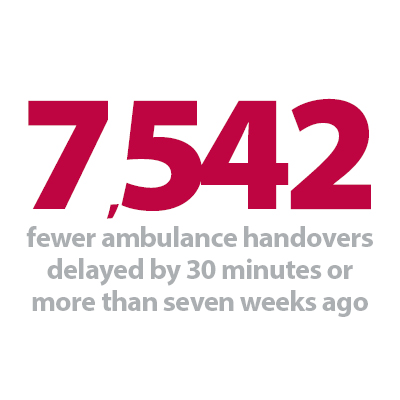
In the latest instalment of the sitreps, we continue to see many of the patterns observed throughout the 20/21 reporting period. The number of adult critical care beds open and occupied remains far above previous years, but general and acute (G&A) bed occupancy has been below the normal headline rate all winter. Compared to a normal winter, there have been far fewer long stay patients and beds closed due to diarrhoea and vomiting (D&V), and norovirus. Ambulance arrivals and handover delays are also considerably lower than usual, in large part because of the extended lockdown.
Key headlines from the latest data:
COVID-19 context:
- The number of COVID-19 patients in hospital (on 3 March) is 9,594, which is 26% fewer than a week ago (3,451 fewer patients). The last time the total was this low was 1 November, which means there have been more than 10,000 patients for the last 121 days.
- The number of COVID-19 patients in mechanical ventilation beds also continues to fall, now 22% fewer than a week ago. The current total of 1,507 is 60% lower than the peak figure reached on 24 January (3,736).
Winter sitreps:
-
The number of adult critical care beds open continues to gradually fall, now 5,310 on average per day. This means that trusts had 5.2% fewer open than last week (291 fewer on average each day), but this remains 44.8% higher than the same time last year (1,643 more beds open).
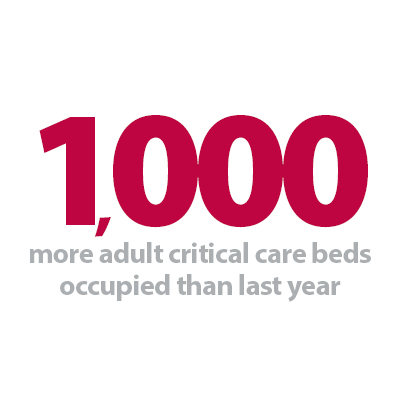
- The number of adult critical care beds occupied fell slightly faster this week (down 7.8%, 337 fewer patients on average each day). However, there were still 3,997 patients in these beds each day, which remains 33.3% more than the same time last year (1,000 more patients).
- Putting these two together, this means the occupancy rate of critical care beds this week is down to 75.3% (from 77.4% last week). At the same point last year, occupancy was 81.8% (although with far fewer beds open).
- National G&A bed occupancy rose slightly again this week (now 85.8%, up from 85.2%), while the total number of beds open was steady at just under 90,000 (0.2% higher than last week, 161 more G&A beds open).
- The number of ambulance arrivals fell slightly this week after a sizeable jump last week. This week, 88,075 patients arrived by ambulance, or 12,582 per day, which is 2.6% fewer than last week.
- Handover delays improved accordingly, this week 8.2% of arrivals were delayed by 30+ minutes (down from 9.5% last week) and 1.8% were delayed by 60+ minutes (down from 2.1%).
Throughout the winter, trusts have had to adapt in a number of ways to the rapidly changing demands of the pandemic. It is true that non-COVID activity in some settings has fallen during the second wave, but far more patients across the board continue to be seen compared to the first wave. At the same time, demand from COVID-19 patients has reached unprecedented levels over the winter, and the response from the NHS has been truly remarkable.
Between the start of December and the end of February, there have been over 1.96 million NHS bed days due to COVID-19 patients. While the first wave saw many new challenges being tackled for the first time, less than half the equivalent total number of bed days due to COVID-19 patients were recorded between the start of April 2020 and the end of June (0.89 million for the 90 days from 31 March when the number of COVID-19 patients in hospital passed 10,000 for the first time).
A particular point of pressure has been in critical care, where trusts have opened far more beds to care for those patients with the most severe illness. Since the start of January, we have seen 56% more of these beds open than last winter, and a very similar number of these have been occupied as soon as they were made available (57% more patients in these beds than last year).
Trusts have gone to great lengths to accommodate and care for these patients, while at the same time working hard to maintain non-COVID services and prioritise patient flow throughout the system. G&A bed occupancy has remained lower than previous years throughout the winter, but as acknowledged, the headline rate will feel far busier on the ground due to the demands of the pandemic, including additional infection protection and control measures. It is a testament to the planning and preparation that trusts undertook ahead of winter that areas of concern in previous years such as high numbers of long-stay patients or lengthy ambulance handover delays have been less of an issue this year.
As we move out of the winter reporting period, trusts would typically expect to be looking ahead and planning how to tackle backlogs in other areas of care. However, with the impact of the virus still being felt across hospitals, ambulance, mental health and community services, the NHS has much to consider in the coming weeks and months. The wellbeing of staff is a top priority for health leaders as they continue to care for both COVID and non-COVID patients, as well as driving the impressive vaccine roll-out that is providing so much hope for the future.
This week’s Winter Watch contribution is from Simon Barton, chief operating officer at Sherwood Forest Hospitals NHS Foundation Trust. He talks about the challenges faced by staff during winter, and how they have been supported. He also highlights the extra measures taken by the trust to manage the rise in demand such as expanding critical care capacity by 300%, reconfiguring admissions pathways and working collaboratively.
Supporting staff has been a key driver this winter and throughout the COVID-19 pandemic
Simon Barton, Sherwood Forest Hospitals NHS Foundation Trust chief operating officer reflects on their experience this winter.
We might be nearing the end of winter sit reps to NHS England, but that doesn’t mean that winter is over for the NHS. As a chief operating officer, my seasons are a bit like Narnia. Winter starts sometime in October and doesn't really end until we see the end of April. The pressures remain high throughout and obviously this winter has been staggeringly difficult.
Like every winter our colleagues have been incredible and awe-inspiring throughout; hard working, flexible, dedicated and remarkably resilient. However, we have really worried for them this year, both in terms of workload and their well-being. Supporting them has been a key driver throughout our COVID response and it has never been far from our minds. It has been a golden thread that we keep returning to as a leadership team – our job is to look after the people who look after the people.
We have put a package of measures put in place to support colleagues, but there are some things that we just can’t fix. We can't fix the loss that people saw every day, we can’t take away their trauma, and we can't fix the fact that we have been living and working with this virus for a year.
It doesn't help that we find both their personal and professional lives are dominated by COVID and it is hard for colleagues not being able to socialise outside of work and debrief over a cuppa or something stronger. These social debriefs are important and spending time with others who have been through the same experiences helps people to deal with what they have been through.
Looking after our colleagues has been instrumental in helping us to respond effectively to the pandemic, but another key has been to remain flexible and agile, enabling us to change to meet ever changing demands. We meet daily as a senior team across all disciplines to make sure that any blockers or issues are dealt with quickly and to allow us to make swift, data led decisions that keep our hospitals working effectively.
For example, we have had make more changes than ever to our ED pathway, all whilst opening up more capacity than we ever thought would be possible or necessary.
We have surged our critical care level to three times its establishment, using both theatres and recovery at our main site, Kings Mill Hospital (KMH). We have managed to keep an elective list going at our other site, Newark, which has been incredibly important to those patients waiting for surgery and have done some limited surgery at KMH.
But this really is a team game. We have been working closely as a system and with colleagues from primary care, the mental health trust, ambulance trusts and councils to ensure that our patients have the right care in the right place. I am very proud of the work in partner organisations which has seen innovations like the establishment of virtual wards external to the hospital, and also of the day to day commitment from our ambulance trusts which sees ambulances continually turned around at remarkable speed.
One reason that this winter has been so exhausting is because you are always balancing risks; containing cross infection with ensuring beds available, whilst constantly recalibrating and trying to fix an ever changing set of issues.
Colleagues describe getting admissions right as a giant jigsaw puzzle with lots of variables. Before COVID it was 1000 pieces, with a clear picture to follow. Now it is a 3D puzzle and getting it right takes time. It isn't because of the number of people coming into hospital, it's the complexity of managing them appropriately.
In fact, in terms of numbers we have seen 5% fewer patients this winter than last, but those we have seen have been much, much sicker and our acuity has been higher than we have ever seen before.
We are now beginning to see a consistent drop in the numbers of COVID patients on our wards, thanks to a combination of lockdown, social distancing and the vaccine. I see this as a glimmer of light that we are getting through this, but COVID isn't going to go anywhere any time soon and it will be a long time before hospitals return to normal.
Before we move on to the next phase we also need to think about colleagues across the NHS and how they can get some time, space and rest so that they can tackle the challenges ahead. Some colleagues are desperate to start work on their 'day job' after a year of change and upheaval but others need time to reflect, to process what they have been through and to recover and recharge.
My job is to continue to work to ensure that colleagues have everything they need to be able to deliver great care, whilst also starting to plan for what comes next and to think about how our services recover, as well as our colleagues. We know that we have another mountain ahead of us once winter is over and now is the time to start charting the course that will see us ready to tackle the climb, with a clear route map to guide us along the way.
Progress is being made, but the NHS is still in stormy waters
Responding to the latest winter reporting data, from NHS England and NHS Improvement, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"We welcome the news that there are now fewer than 10,000 COVID-19 patients in hospital for the first time since early November. We are seeing signs that those who received an early vaccine are now less likely to become seriously ill from the virus, but we know that younger age groups continue to be affected in high numbers. The overall number of patients in critical care is still more than 30% higher than at the same point last year.
"Inevitably, as the immediate pressures from COVID-19 recede, there is a growing focus on the challenges ahead including the need to tackle backlogs in other areas of care. But we're still seeing the impact of the virus across hospitals, ambulance, mental health and community services. Staff continue to don cumbersome PPE, and many continue to be redeployed or absent from work due to illness or isolation. It's important that additional infection prevention control measures remain in place, but that means NHS capacity to get going with other work is constrained.
"The priority of trust leaders is the wellbeing of their staff, who working tirelessly to look after both COVID and non COVID patients, and are rolling out the vaccination programme. We urge the government to maintain a cautious approach if this is to be the last lockdown. We must build on the progress made, recognising we are still in stormy waters, with the NHS operating under more pressure, and with less capacity, than usual."