

Today saw the second week of the winter sitreps published by NHS England and NHS Improvement. Developments in the COVID-19 pandemic continue to impact trusts, and this week several areas of concern are starting to emerge in the winter data.
For several weeks the number of cases of the virus had been falling nationally, but the latest week saw a considerable increase in both new cases and hospital admissions, with areas in the south of the country particularly affected. The additional demands of COVID-19 and the need for social distancing and infection prevention and control mean all care settings feel busier. The sitreps data published today give an indication of the current pressure on trusts.
Key headlines from the winter sitreps (7 – 13 December):
- there were 44 A&E diverts this week, the highest weekly figure seen across the last three winters and very unusual so early in the season
- ambulance handovers worsened this week, with 14.5% of all patients arriving by ambulance delayed by 30 minutes or more (up from 11.0% last week)
- general and acute bed occupancy was up by almost two percentage points to 88.9% this week (87.1% last week)
- we continue to see far fewer patients staying in hospital longer than 7, 14 and 21 days compared to previous years
- the number of beds closed with diarrhoea and vomiting (D&V) and norovirus remains very low, with an average of 50 closed per day this week (down from 58 last week).
While it is useful to consider the national picture, we know that the COVID-19 situation is constantly changing on a regional and local level, and as a result the specific pressures on trusts in different parts of the country will vary. The high number of A&E diverts was centred on a small number of locations, and for these health and care systems the last week will have been particularly tough. Action plans to tackle the pinch-points will be deployed, and all trusts will be looking to take pre-emptive action to avoid these events as far as possible in the future.
The ambulance figures this week indicate similar pressures. The overall number of patients arriving by ambulance this week was consistent with the previous week, but there were an additional 3,000 patients whose handover was delayed by 30 minutes or longer compared to the previous week. Worryingly, within this group there was a large increase in those waiting 60 minutes or longer, with 75% more people enduring these long waits than in week 1.
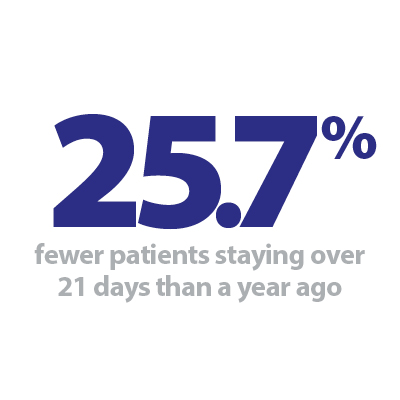
Bed occupancy increased from 87.1% to 88.9% this week, and while this remains significantly lower than the same time last year, this will feel much busier for trusts as they juggle the demands of treating COVID-19 patients as well as their own workforce and resource constraints. On a positive note, the number of long-stay patients is well below the level seen in previous years, with 16% fewer staying over seven days, 22% fewer staying over 14 days and 26% fewer staying over 21 days than at the same time last year. Also, the impact of D&V and norovirus remains exceptionally low, and with only a small number of incidences of seasonal flu reported, trusts will hope for these levels not to rise in the weeks to come.
This week, our featured contribution takes the form of an NHS Providers podcast, as Adam Brimelow, director of communications, leads a conversation with Claire Helm, senior analysis manager and Julian Russell, senior research analyst, about what trusts can expect over the coming winter months, the impact of COVID-19 and statistics from the first week of Winter watch.
Winter Watch: Breaking the ice
The Provider Podcast Season 3: Episode 1
Welcome to The Provider Podcast from NHS Providers. Adam Brimelow leads us through our three part podcast series, alongside our #NHSWinterWatch campaign, for winter 2020/21. Throughout this series we'll be talking to experts in the NHS, including leaders from Care Quality Commission, about what winter holds for the NHS.
In this live virtual recording, we have a quick chat with experts from our very own NHS Providers analysis team, Claire Helm and Julian Russell, about what trusts can expect over the coming winter months, the impact of COVID-19 and statistics from our first week of #NHSWinterWatch.
Winter data shows a picture of growing pressures
Responding to the latest winter reporting data, from NHS England and NHS Improvement, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"This week's performance statistics show just how hard trusts and staff are working amid extremely challenging pressures.
"We are deeply concerned that this week there were 44 A&E diverts, higher than anything we've seen across the last three winters and unusual so early in the season. These diverts are a result of localised pressures, indicating that some health and care systems are struggling with the number of patients who need their help.
"Despite best efforts by paramedics and hospital staff, this picture of growing pressure is also reflected in the worsening of ambulance handover times in the past week. Separate data shows that 21% more people were admitted to hospital for COVID-19 this week than the week before.
"While the data highlights that headline bed occupancy is better than last year, we know that with the additional demands of COVID-19 and the need for social distancing and infection, prevention and control, all care settings will feel busier for trusts. It is concerning to see this figure increasing so soon when we are yet to see any major flu outbreak, a cold snap or a D&V outbreak.
"On a more positive note, there have been far fewer patients staying longer than 7, 14 or 21 days in hospital compared to last year, and very few beds closed due to norovirus.
"Staff are continuing to go above and beyond to keep patients safe, but we are increasingly concerned that should pressures continue to rise throughout the festive period, trusts, their staff and patients may face an incredibly challenging start to 2021."