There are major opportunities to transform the NHS estate to become more sustainable, efficient and digitised. Trust sites designed to support new models of care, digital transformation and clinical research have the potential to lead to measurable improvements in key health outcomes. Indeed, the NHP has the capacity to improve patient-centred care and experience, drive long overdue improvements in patient safety, materially improve staff recruitment and enable trusts to increase productivity.
This section considers the scope of wholescale transformation of the NHS estate, how capital investment can underpin major changes to service delivery, and with the right support from government, can enable trusts to maximise economic and social value from its estate and use it more efficiently.
Capital investment vital to enable NHS to deliver on net zero ambitions
The NHS plans to become the world’s first net zero carbon national health system. As part of its strategy, the carbon footprint of emissions it controls should be net zero by 2040. Systems are therefore expected to consider the impact of capital spending on trusts' carbon footprint, local air pollution, and the health of staff and patients.
As well as reducing the carbon impact of major infrastructure projects like building new hospitals, there are sustainable day-to-day changes that can reduce the NHS’ carbon footprint. However, major investment is required to improve energy efficiency across the NHS estate and enable trusts to reduce their carbon footprint.
Significant funding was announced at the SR to decarbonise the NHS. Like other public sector bodies, NHS trusts and foundation trusts may apply for funding via the Public Sector Decarbonisation Scheme operated by the Department of Business, Energy and Industrial Strategy (BEIS). The scheme takes a ‘whole building approach’ to decarbonising heat. Current projects include the installation of air and ground source heat pumps; improving energy efficiency through double glazing, loft and cavity wall installation; installing LED lighting, and setting up solar panels to produce renewable electricity.
This financial support has enabled some trusts to materially progress their net zero strategies. As NHS Providers noted in our report on trusts’ efforts to reach net zero emissions, as well as transforming supply chains and enabling more sustainable procurement strategies, the route to large-scale decarbonisation will also require significant capital investment. For example, enabling the NHS to transition to a fully zero emission ambulance fleet will require investment in the wider NHS estate to provide electric vehicle charging stations.
However, the financial case for transformative 'green plans' can be challenging when annual capital charges exceed cost savings. In addition, given the limited headroom across the NHS capital budget, it is unclear whether the main source of funding going forward will be via BEIS rather than DHSC.
Delivering fully digitally connected estates
Capital investment to improve interoperability
Frontline digitisation via electronic patient records (EPRs) has long been identified as a key enabler in transforming services to improve outcomes, tackle inequalities, enhance productivity and contribute to broader social and economic development. This is relevant for both new builds and estate refurbishments.
Trusts require the 'basics' to be right first, ensuring they have a strong foundation to grow their digital maturity – including reliable Wi-Fi coverage, strong technical infrastructure, and EPRs – before moving ahead to any more advanced digital health technologies. Digital needs must therefore be considered at the outset when designing new hospitals.
As NHS Providers’ Digital Boards programme has evidenced, EPRs can enhance patient safety by enabling synchronous data entry at the point of care; improve staff satisfaction by transforming the usability of software; increase productivity by reducing the time spent by staff entering and searching for data, and help inform service transformation to improve population health management.
Interoperability and the ability of technical systems to exchange information across organisations and systems is vital. As the BMA highlights, improving the level of coordination between primary and secondary care is vital to reducing the care backlog by helping to speed up clinical and administrative processes, and ensuring patient pathways are completed as quickly as possible.
The need for a long-term view of benefits realisation from digital investment
Trust leaders welcomed the £2.1bn of capital funding allocated at the SR to improve NHS technology and digital assets. However, the current level of digital investment is not enough to support trust leaders to meet the ambitious digital transformation goals set out in DHSC’s digital strategy for health and social care. There remain concerns that digital investment will be scaled back at a time when trusts and systems require these enablers to deliver long-term transformation of the estate. It is also important for policy makers to explore a rebalance of the funding model for digital, which requires both revenue and capital investment.
The government must take a long-term view on digital funding. It can take 5-10 years for the benefits of digital transformation to be fully realised. For this reason, constantly changing, short-term national digital priorities hamper trust leaders' ability to build digital foundations for the long term.
New Hospitals Programme
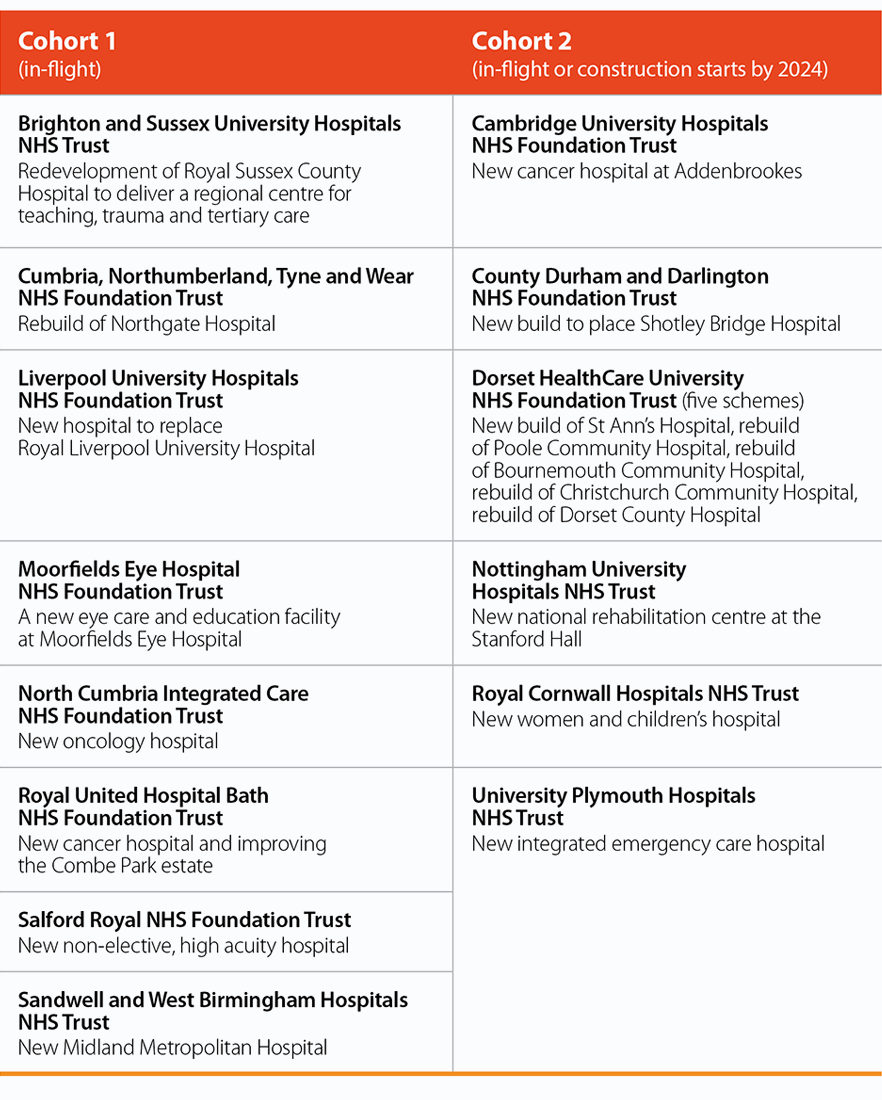
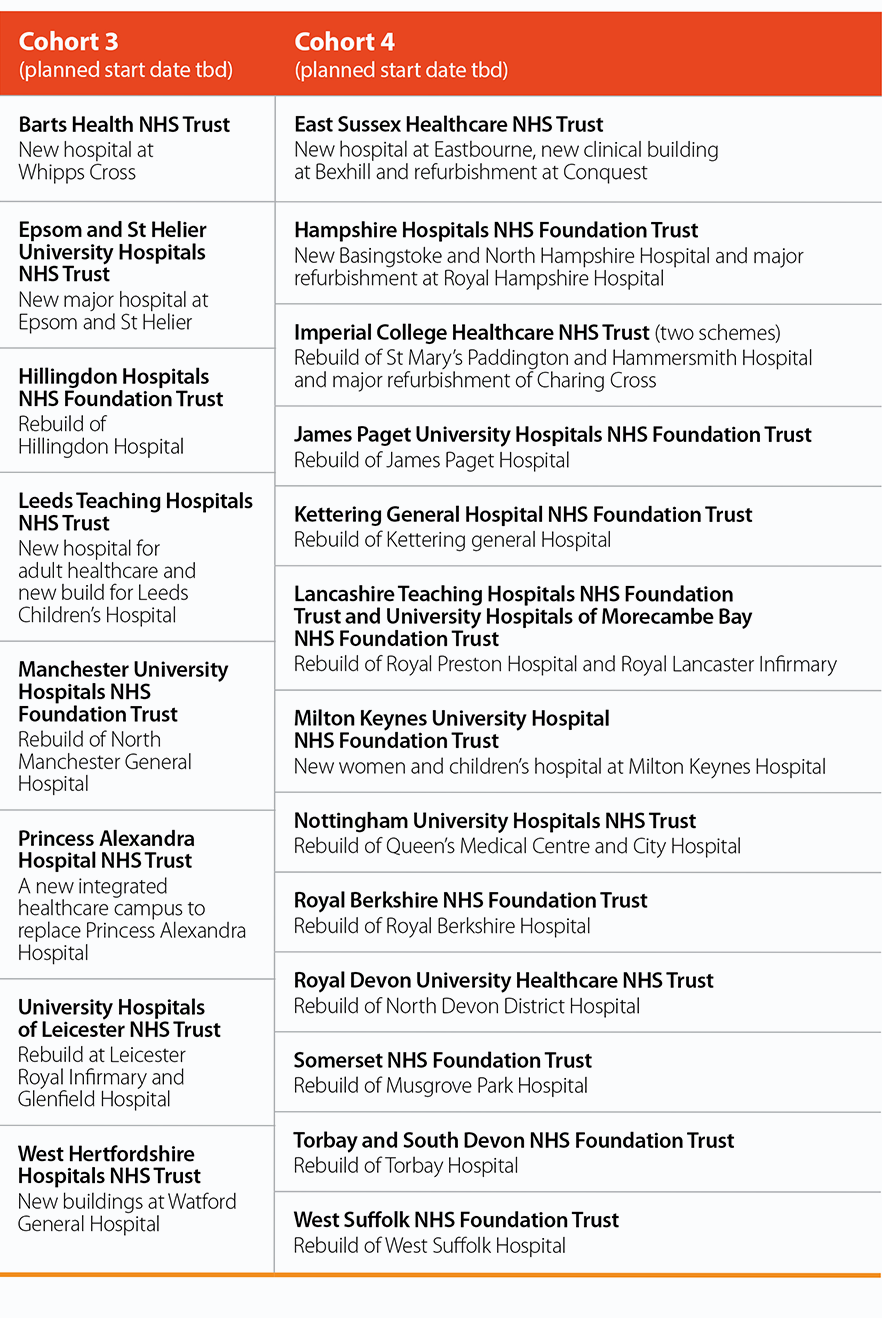
In September 2019 the government launched the Health Infrastructure Plan (HIP), which announced funding for six new hospitals and seed funding for an additional 21 trusts to develop business cases for proposals. The Conservative Party’s 2019 manifesto committed to building 40 new hospitals by 2030. In October 2020, the then prime minister announced the trusts that comprise the New Hospital Programme (NHP). This included the initial six HIP1 trusts. Some of these projects were already in flight. There are currently 40 separate projects across 35 trusts in the programme, and their business cases are at different stages of development.
In July 2021 the government announced it planned to fund an additional eight hospitals. Trusts which applied to be included in the final cohort are still awaiting the outcome of the selection process.
Trusts and foundation trusts currently in the New Hospital Programme
Is there enough funding to meet the ambitions of the programme?
Given that many parts of the NHS estate are in extremely poor condition, in some cases, demolition and rebuild is the only viable way forward. As highlighted in section four, some trusts' critical infrastructure risk can become increasingly costly and operationally challenging to mitigate. New builds can therefore enable trusts to significantly reduce their maintenance backlog by repurposing, refitting or replacing outdated facilities.
In October 2020 the prime minister announced that £3.7bn would be made available for trusts to make progress on the 40 hospitals across all cohorts, and at the SR the government confirmed this funding for 2022/23 to 2024/25. The current envelope therefore does not cover the life cycles of all the projects. Additional funding was also made available for upgrades at trusts outside of the NHP.
While the initial £3.7bn of investment between 2022/23 and 2024/25 was welcome, it is unclear how far this notional capital envelope will enable trusts to deliver at their preferred scale – particularly as demands on this budget for those trusts currently in the programme continue to grow. Trusts have identified the financial cost of delays given inflationary pressures across the construction sector and material inputs. It is unclear whether there are any plans to announce a revised budget for the NHP beyond the spending review period.
The challenge in aligning local plans and business cases with a national programme
The NHP has also highlighted the tension in delivering a national programme driven by the government with individual trusts which remain accountable to and close to their local populations. The programme ultimately requires co-design between national government and local and regional health systems.
The NHP has been delayed as central government seeks to agree a programmatic approach to delivery, and because the projects were all at different stages of business case development when the NHP was announced. Some are still at the first stage (strategic outline case) which assesses the initial scope of the project; others have moved on to the second stage (outline business case) which sets out the preferred option and determines affordability and funding requirements.
There is buy-in to the programmatic approach given its economic and social value, and its potential to benefit all constituent trusts currently part of the NHP, as well as trusts that will utilise the capability and capacity of the NHP in the future. However, trusts are still waiting to proceed pending funding approval.
What is the value of design standardisation and what are the costs?
The NHP is expected to transform the procurement and design strategy for manufacturing material inputs for new hospitals. A standardised approach means it should become cheaper in the longer term to build hospitals and enable more efficient use of trusts' estates. Modern methods of construction (MMC) is a now a key policy of the government and the NHS, with a national target for NHS capital projects over £25m to deliver MMC for 70% of new builds and 50% for refurbishments.
It is unclear at this point how many trusts currently part of the NHP will be expected to employ MMC. Trusts recognise the value of MMC in reducing long-term delivery costs and how design standardisation can improve clinical outcomes. There may be however major cost implications to implementing full standardisation in the short term.
Strategic use of the NHS estate: partnerships with communities, research and industry
The government should continue to explore how the NHS can maximise values from land disposal and use the wider estate more efficiently for the benefit of staff, patients and communities.
The value of land and buildings owned by NHS providers stood at £38.2bn at the end of 2020/21. The Naylor review explored the value in releasing inefficient or unused land that was no longer needed for the delivery of healthcare. The commission estimated that land disposal across the acute and non-acute sectors could release risk-adjusted capital receipts with a value of £2.7bn – this figure could be higher if the NHS were able to secure more cost-effective housing quotas and develop a more commercially orientated approach to estate management, and if planning regulations were more amenable.
Anchor capital strategies to benefit communities
Trusts play a key role in creating economic and social value for their communities – as a major employer, a provider of key services and advice and often as a supporter of local businesses and voluntary sector organisations. This is particularly important for rural providers where there are few other public service institutions which have the capacity to play a similar role.
The Naylor review identified opportunities to develop affordable housing models for NHS staff in collaboration with housing associations and developers.
The Health Foundation has also outlined how ‘anchor capital strategies’ can operate in practice, expanding community access to the NHS estate, converting land using capital receipts for the benefit of local communities, and improving staff wellbeing and retention by developing more affordable housing.
Land disposal and partnership with the life sciences industry
Some trusts have been developing bids for clinical and research facilities for additional bed capacity, as well as life science clusters, which are developed (and funded) through partnerships with industry. Policy makers should explore the scope for further partnerships between NHS organisations with the life sciences industries to enable trusts to improve their estate and patient care, while also investing in vital research and development.
Trusts are now able to generate 'CDEL 'credits' through land disposal, which means the credit from land and property does not have to be used in the same year, and could help enable greater flexibility over their multi-year capital spending profile. However, there are limitations on any sales from land disposal, as any profits above the net book value of assets must remain affordable within system envelopes.
Primary care estate
While the focus of this report has centred on secondary care, it is also vital to consider the recommendations of the Fuller stocktake of primary care. The report noted that GP owner-occupied
models can limit cross-system working and estate management, and that ICSs should ensure system estate transformation plans take due consideration of population health, access and inequalities.