

Introduction
Today the weekly winter situation reports by NHS England were published, providing an insight into the situation on the ground from 6 to 12 February.
The improvements in the data this week continue to show how trust staff are working extremely hard to keep up with the high demands and seasonal pressures, particularly during one of the toughest winters for the NHS.
Winter situation report (6 February – 12 February)
A&E closures and diverts: There were no A&E closures again this week. There were a total of 9 A&E diverts, eight fewer than the week prior.
Adult critical care: Adult critical care bed occupancy dropped this week to 78.0%, down from 79.4%. However, this is still above levels seen in the same week last year (75.3%).
Ambulance arrivals: A total of 78,241 patients arrived by ambulance. This is a decrease of 2.8% since last week and down by 8.5% compared to the same week last year.
Ambulance handovers: 20% of ambulance handovers were delayed by 30 minutes or more, down from 23.6% last week. 6.8% were delayed by 60 minutes or more, this is down from 9.6% last week. A total of 10,186 hours were lost to ambulance handover delays.
Diarrhoea and vomiting: The number of beds closed due to diarrhoea and vomiting and norovirus has decreased slightly this week, with an average of 896 beds closed per day. This is down from 915 last week but remains considerably higher than this time last year (226).
Discharges: There were an average of 23,151 patients each day who no longer met the criteria to reside, a decrease of 621 patients from the week prior. However, compared to last week, a slightly higher proportion of patients remained in hospital this week, with 69.1% (or 13,498) staying in hospital.
Flu: This week the average number of general and acute (G&A) beds occupied by flu patients each day decreased by 23% to 687. An average of 50 critical care beds were occupied by flu patients each day this week (24% fewer than the week before). Compared to the same week last year, the average number of G&A beds occupied by flu patients each day has increased by 2,603% (662 more). The average number of critical care beds occupied by flu patients has increased by 2,100% from the same time last year (48 more).
G&A: There were an average of 100,855 G&A beds open each day – 3.9% higher than the same time last year (3,787 more). On average each day, 322 beds were unavailable and void to non-COVID infections. Average bed occupancy remains high at 93.8% but is down from last week (94.4%). This is 1.5 percentage points lower compared to the same week last year.
Long stay: The number of patients staying in hospital longer than seven, 14 and 21 days has continued to fall this week, down by 0.2%, 0.2% and 1.2% respectively. However, compared to the same time last year, the numbers of patients staying in hospital for longer than seven, 14 and 21 days have all increased (up by 10.0%, 11.9%, and 12.2% respectively).
Neonatal intensive care unit: Occupancy has fallen this week to 65.3% compared to 66.8% last week, and down from 65.7% the same week a year before. The average number of care beds open is at 1,695, 1% more beds open compared to last year.
Paediatric intensive care unit: Occupancy has fallen this week to 81.4% (it was 83.5% last week) However, this is still higher than the same week last year (72.4%). The average number of care beds open has fallen by four beds to 355.
Respiratory syncytial virus (RSV): An average of 23 paediatric beds were closed this week due to RSV symptoms, slightly down from 25 last week but up considerably from 5 last year.
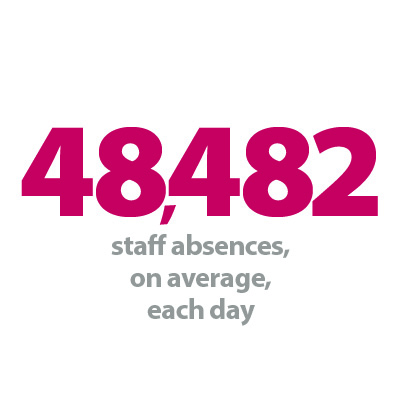
Staff absences: There were an average of 48,764 total absences each day this week, of which 10% were COVID-19 related (4,714). The total number of staff absences decreased from the week before (49,333) but the number and proportion of COVID-19 related absences both increased.
Our view
This week's data show the ongoing efforts from staff to meet the needs of their patients during a remarkably challenging time for the NHS.
There was some respite, however, with fewer ambulance handover delays this week. We also saw a reduction in neonatal intensive care unit and paediatric intensive care unit bed occupancy, and in the number of beds occupied by flu patients.
That said, general and acute and adult critical care bed occupancy levels remain worryingly high, with the former at around 94%. Equally, a higher proportion of patients continued to stay in hospital when medically fit to be discharged, a sign of the system wide pressures felt across the health and care sector.
Nested winter discharge ward
Eilish Midlane, chief executive at Royal Papworth Hospital NHS Foundation Trust, talks through a pioneering partnership which has seen them set up a nested ward in collaboration with Addenbrooke's Hospital.
Since the start of the year, patients who are medically fit for discharge are being looked after in a new nested ward – a temporary ward created within another trust.
The two trusts involved – Royal Papworth Hospital NHS Foundation Trust (RPH) and Cambridge University Hospitals NHS Foundation Trust (CUH) – are located next to each other on the Cambridge Biomedical Campus and are joined by an underground tunnel.
The nested ward has been set up by teams at Royal Papworth to help ease winter pressures at CUH, particularly while there is such high demand for emergency care.
After weeks of planning, the 20-bed ward was opened in early January and will remain open until the spring, housing CUH patients who are medically fit for discharge but awaiting a care package.
Staffed by CUH nurses and healthcare support workers, with support provided by RPH catering, digital and estates teams, the ward discharged 87 patients in the first month of being open, with 106 patients cared for in total.
The average length of stay has been 4.7 days.
RPH created the space for its neighbours by temporarily re-locating the non-clinical services normally based in the ward – such as education and PPE teams – which means it is having no impact on RPH's own clinical capacity, while at the same time boosting CUH's.
This has freed up beds at Addenbrooke's, allowing them to ease pressures with patient flow coming through from their emergency department.
The NHS is facing significant pressure nationally and locally. Here in Cambridgeshire and Peterborough, we have come together effectively as an integrated care system this winter, with the NHS, social care and local authority all coming to the table to ensure the best possible care for patients.
This nested ward is just one example of collaborative working and was something I have been keen to establish to help our system partners.
Of course, there were many challenges to overcome, such as deciding which patients would be most suitable to be moved, having different digital systems and electronic patient records across the two trusts, familiarisation training for our CUH colleagues and re-homing our RPH teams who were in this ward.
But we have collectively shown it is possible and it is making a difference.
By creating this extra capacity, it has helped get patients out of ambulances at A&E and into beds, enabling more patients to get the care they need this winter.
Kirsty Jones, the CUH matron on the new ward said:
"Royal Papworth has made us feel really welcome and we're making good progress in discharging around three or four patients every day.
"Our focus on this ward is to make sure patients are enabled to do things for themselves and to improve their mobility as much as possible.
"Getting patients back home or to a care home is vital for easing pressure on beds in Addenbrooke's but it's also better for patients. Staying in hospital can increase the risk of infection and deconditioning so staying active and returning to daily routines at home is really important."