

Introduction
Our NHS Winter Watch 2022/23 series concludes today following the release of this week's winter situation report data from NHS England.
Today's data were published alongside the monthly performance and activity statistics. As always, these provide a valuable insight into the situation on the ground as trusts continue to work tirelessly to deliver an ambitious catch-up plan while dealing with demand, system wide pressures and workforce challenges.
Key points from the performance and activity statistics include:
Ambulance activity: February saw a decrease in both category 1 and 2 incidents, but the average response times for calls are still missing the targets.
Emergency care activity: A smaller number of A&E attendances (1.91 million) were registered in February, as well as fewer emergency admissions, but performance has not met the targets. However, the number of patients waiting more than 12 hours from the decision to admit to admission has decreased again by 18%.
Elective care: Activity has increased across the board in January, but the waiting list remains high at 7.2 million. That said, those waiting more than 78 weeks has decreased this month and this figure is now at 45,631.
Cancer: Activity remained above pre-pandemic levels for all pathways in January and performance against the waiting time standards has improved for the two week pathway. The NHS is however still missing all key national targets.
Diagnostics: There was an improvement in activity registered in January, with almost 2.2 million diagnostic tests carried out, a figure above pre-pandemic levels. That said, the waiting list remains high at 1.5 million.
Urgent community response: As of January 2023, eight in 10 urgent community response referrals met the two-hour standard.
Mental health: Referrals dropped in December but continue to be higher than before the pandemic. However, there were more people in contact compared to the month before, a figure also greater than before the pandemic.
Winter situation report (27 February – 5 March)
A&E closures and diverts: There was one (1) A&E closure this week, the only one this winter season. There were a total of 11 A&E diverts this week, 18 fewer than the week prior.
Adult critical care: Adult critical care bed occupancy increased this week to 78.7%, up from 78.4%. This is also above levels seen in the same week last year (74.9%).
Ambulance arrivals: A total of 79,735 patients arrived by ambulance in the latest week. This is an increase of 1.5% since last week and down by about 5% compared to the same week last year.
Ambulance handovers: 23.3% of ambulance handovers were delayed by 30 minutes or more, slightly down from last week. 9.3% were delayed by 60 minutes or more, also slightly down from 11% last week. A total of 18,573 hours were lost to ambulance handover delays.
Diarrhoea and vomiting: The number of beds closed due to diarrhoea and vomiting (D&V) and norovirus has increased slightly this week, with an average of 720 beds closed per day. This is down from 710 last week but remains higher than this time last year (330).
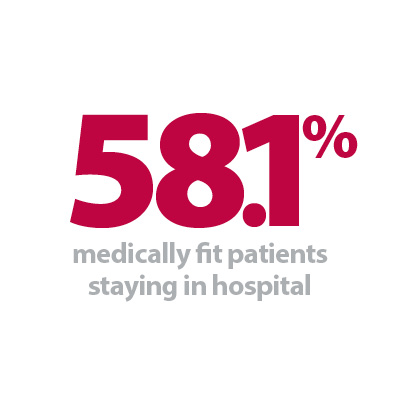
Discharges: There were an average of 22,836 patients each day who no longer met the criteria to reside, a decrease of 750 patients from the week prior. However, compared to last week, a similar proportion of patients remained in hospital this week, with 58.1% (or 13,272) staying in hospital.
Flu: This week the average number of general and acute (G&A) beds occupied by flu patients each day decreased by 18% to 398. An average of 32 critical care beds were occupied by flu patients each day this week (2% fewer than the week before). Compared to the same week last year, the average number of G&A beds occupied by flu patients each day has increased by 722% (350 more). The average number of critical care beds occupied by flu patients has increased by 696% from the same time last year (28 more).
G&A beds: There were an average of 101,029 G&A beds open each day – 3.3% higher than the same time last year (3,239 more). On average each day, 287 beds were unavailable and void due to non-COVID infections. Average bed occupancy increased very slightly to 94.3%. This is an increase of 1.8 percentage points compared to the same week last year.
Long stay: The number of patients staying in hospital longer than 14 days remained somewhat stable (+0.3%). Those staying longer than seven and 21 days remained at a similar level, decreasing by 0.1% and 0.2% respectively. Compared to the same time last year, the numbers of patients staying in hospital for longer than seven, 14 and 21 days have all increased (up by 9%, 11%, and 12% respectively).
Neonatal intensive care unit: Occupancy has fallen this week to 65.7% compared to 66.1% last week, also down from 64.7% the same week a year before. The average number of care beds open is 1,701, 1.1% more beds open compared to the same time last year.
Paediatric intensive care unit: Occupancy has fallen this week to 82.1%, down from 83.0% last week. This remains higher than the same week last year (72.9%). The average number of care beds open this week has fallen by two beds to 355.
Respiratory syncytial virus (RSV): An average of 10 paediatric beds were closed this week due to RSV symptoms, up from eight last week but slightly up from six last year.
Staff absences: There were an average of 48,356 total absences each day this week, of which 11% were COVID-19 related (5,117). The total number of staff absences decreased slightly from the week before (48,497) but the proportion of COVID-19 related absences remained the same.
Our view
This week's data show some signs of improvement, particularly on elective care recovery with an increase in activity and a reduction in the number of patients waiting over 18 weeks. Trusts are doing all they can to meet the next key milestone in the elective recovery plan to eliminate all waits over 78 weeks by April.
We also saw an increase in diagnostics, and cancer activity remains above levels seen before the pandemic. These undoubtedly positive signs are a testament to the hard work of staff, whose valiant efforts all through winter allowed trusts to continue delivering care in the face of numerous challenges.
We are, however, still seeing pressures across the urgent and emergency sector, with figures for ambulance demand and response times somewhat stable, but handover delays continuing to be an issue. Equally, delayed discharges are particularly problematic; once again, a symptom of patient flow challenges across health and social care services. It is worth noting too how mental health demand continues to increase, with more people in contact with services in December, for example.
As the winter period comes to an end, trust leaders are aware of how fragile the road to recovery is. There is a concern that progress could be hindered by both the ongoing pressure from industrial action, which has already seen hundreds of thousands of appointments rescheduled, and existing staff vacancies. Recovery will no doubt require a fully-funded, long-term workforce plan so that the NHS can catch up and thrive.