

Introduction
Today the weekly winter situation reports by NHS England were published, providing an insight into the situation across emergency care and hospitals from 13 to 19 February.
This week's data continues to highlight the pressures that the NHS is under. However, the improvements in the data continue to demonstrate the efforts from staff and trust leaders to keep up with these seasonal pressures.
Winter situation report (13 February – 19 February)
A&E closures and diverts: There were no A&E closures again this week. There were a total of four A&E diverts, five fewer than the week prior.
Adult critical care: Bed occupancy dropped this week to 77.7%, down from 78%. However, this is still above levels seen in the same week last year (75.2%).
Ambulance arrivals: A total of 79,752 patients arrived by ambulance this week. This is an increase of 1.9% since last week, but down by 5.7% compared to the same week last year.
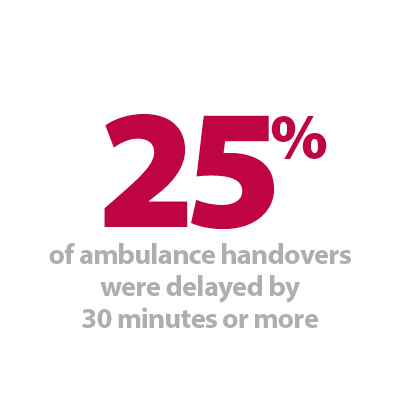
Ambulance handovers: 25% of ambulance handovers were delayed by 30 minutes or more, up from 20% last week. 10.4% were delayed by 60 minutes or more, this is up from 6.8% last week. A total of 17,187 hours were lost to ambulance handover delays.
Diarrhoea and vomiting: The number of beds closed due to diarrhoea and vomiting and norovirus has decreased again this week, with an average of 821 beds closed per day. This is down from 896 last week but remains higher than this time last year (203).
Discharges: There were an average of 23,242 patients each day who no longer met the criteria to reside, a slight increase of 91 patients from the week prior. However, compared to last week, a similar proportion of patients remained in hospital this week, with 58.9% (or 13,694) staying in hospital.
Flu: This week the average number of general and acute (G&A) beds occupied by flu patients each day decreased by 12% to 603. An average of 35 critical care beds were occupied by flu patients each day this week (30% fewer than the week before). Compared to the same week last year, the average number of G&A beds occupied by flu patients each day has increased by 2,169% (576 more). The average number of critical care beds occupied by flu patients has increased by 1,650% from the same time last year (33 more).
G&A: There were an average of 101,067 G&A beds open each day – 3.4% higher than the same time last year (3,330 more). On average each day, 293 beds were unavailable and void to non-COVID infections, down from 322 last week. Average bed occupancy remains high at 94.1%, up slightly from last week (93.8%). This is 1.8 percentage points greater compared to the same week last year.
Long stay: The number of patients staying in hospital longer than seven days dropped slightly this week (-0.5%). However, those staying longer than 14 and 21 days increased by 0.2% and 0.5% respectively. Compared to the same time last year, the numbers of patients staying in hospital for longer than seven, 14 and 21 days have all increased (up by 9.5%, 12.0%, and 13.0% respectively).
Neonatal intensive care unit: Occupancy has fallen slightly this week to 65.1% compared to 65.3% last week, and down from 66.7% the same week a year before. The average number of care beds open is at 1,703, 0.6% more beds open compared to the same time last year.
Paediatric intensive care unit: Occupancy has fallen this week to 80.1%, down from 81.4% last week. However, this is still higher than the same week last year (68.7%). The average number of care beds open this week has risen by eight beds to 363.
Respiratory syncytial virus (RSV): An average of 16 paediatric beds were closed this week due to RSV symptoms, down from 23 last week but up considerably from eight last year.
Staff absences: There were an average of 48,269 total absences each day this week, of which 10% were COVID-19 related (4,987). The total number of staff absences increased slightly from the week before (48,269) but the proportion of COVID-19 related absences remained the same.
Our view
This week's data continues to highlight the ongoing efforts from staff and trust leaders to meet the needs of their patients, despite the system wide pressures being felt across the NHS.
There were some improvements in the data with fewer beds occupied by diarrhoea and vomiting, norovirus and flu patients. We also saw a reduction in adult critical care bed occupancy this week, but this remains higher than the levels seen at the same point last year.
Furthermore, bed flow continues to be a challenge for the NHS. G&A bed occupancy levels remain extremely high at 94%, as is the number of delayed discharges with 13,700 patients remaining in hospital when medically fit to be discharged. We have also seen a rise in ambulance handover delays this week which reflects the intense demand trusts are facing right across systems, both in, and outside hospitals.
If you can't make your appointment – 'pass it on'
Jane Harris, associate director of communications and partnerships at Torbay and South Devon NHS Foundation Trust discusses the organisation's 'pass it on' campaign which highlights the importance of reallocating appointments to other patients when a patient can no longer attend.
In January, Torbay and South Devon NHS Foundation Trust (Torbay and South Devon) launched a campaign to ask for local people's help with letting the organisation know if they can't make their appointment. This was in order to make sure people are getting the care they need as quickly as possible.
Across the NHS, teams are very aware of the impact that missed appointments can have, both financially and on the delivery of care. Torbay and South Devon wanted to reinforce the message to its communities to please get in touch if they can't make their appointment.
Of the 122 million appointments booked last year (2021/22) across NHS trusts in England, around 6.4% were missed – around 7.8 million appointments a year and around 650,000 a month.
At Torbay and South Devon, endoscopy services were identified as a particular issue as, due to the preparation required ahead of appointments, these slots aren't able to be rebooked quickly and need four-to-five days' notice.
Our teams are aware that there are many reasons why people can't make their appointments, and we will always do our best to be flexible to people's circumstances. It is really important that people let us know so that their appointment can be rearranged, and the slot can be reallocated. Ensuring that every appointment is taken up is part of wider work around tackling waiting lists nationally. It also supports the delivery of care, as reassurance is provided, care received or treatment started much sooner.
The 'pass it on' campaign asks members of the public to get in touch if they can't make their appointment as soon as possible; so that this can be both rearranged and offered to another person waiting for care.
Data from January outpatient activity was used to set a benchmark for improvement. Over 1,800 outpatient appointments in January were not attended amounting to just over 4% of all outpatient appointments.
Press activity complimented social media graphics and posters with the key messages of the campaign;
- "Can't make your appointment? Give it to someone who can"
- "By letting us know you can't make it, we can offer your appointment to someone else who is waiting. Please pass it on."
By providing a clear call to action and an added benefit that the appointment can be allocated to someone else waiting, the campaign aims to speak to members of the public directly and highlight the consequences of not letting people know.
A clear connection has been made by the campaign to the elective recovery programme and the benefit of passing on appointments for the next person who is waiting to be seen. Current pressures on the NHS are well documented and the campaign highlights that we all have a role to play in reducing waiting times and waiting lists.
Although the campaign was only recently launched, it is hoped that the impact of helping people feel more comfortable in notifying and cancelling will have a demonstrable effect on attendances and prior notice.