
Introduction
Another release of the weekly winter situation reports was published by NHS England today, offering a snapshot of activity on the ground as trusts continue to work hard to meet demand.
This week's data reflect similar trends observed in previous weeks, although there have been some slight improvements, for example across the ambulance sector. This shows how staff continue to work tirelessly throughout a very challenging winter exacerbated by an earlier surge in flu cases and industrial action.
Winter situation report (23 – 29 January)
A&E closures and diverts: There were no A&E closures again this week. There were a total of 10 A&E diverts this week, nine fewer than the week prior.
Adult critical care: Adult critical care bed occupancy dropped again this week to 79.3%, down from 80.6%. However, this is still above levels seen in the same week last year (74.0%).
Ambulance arrivals: A total of 78,431 patients arrived by ambulance in the latest week. This is a similar number (+0.8%) to last week and a decrease of 8.8% compared to the same week last year.
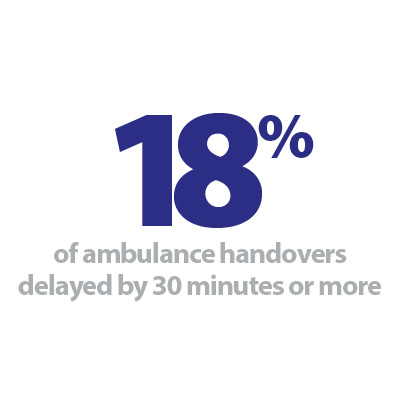
Ambulance handovers: 18.2% of ambulance handovers were delayed by 30 minutes or more, a decrease from 20.2% last week. 5.6% were delayed by 60 minutes or more. This is a decrease from 6.6% last week. A total of 8,899 hours were lost to ambulance handover delays, another decrease from the week before.
Diarrhoea and vomiting (D&V): The number of beds closed due to D&V and norovirus has increased this week, with an average of 495 beds closed per day. This is up from 473 last week and remains above levels seen this time last year (413).
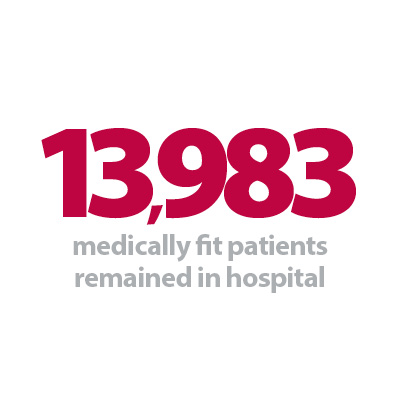
Discharges: There were an average of 23,517 patients each day who no longer met the criteria to reside, an increase of 534 patients from the week prior. However, compared to last week, a similar proportion of patients remained in hospital this week, with 59.5% (or 13,983) staying in hospital.
Flu: This week the average number of general and acute (G&A) beds occupied by flu patients each day decreased by 36% to 1,203. An average of 87 critical care beds were occupied by flu patients each day this week (38% fewer than the week before). Compared to the same week last year, the average number of G&A beds occupied by flu patients each day has increased by 3,324% (1,168 more). The average number of critical care beds occupied by flu patients has increased by 6,689% from the same time last year (86 more).
G&A beds: There were an average of 101,048 G&A beds open each day – 4.2% higher than the same time last year (4,106 more). On average each day, 274 beds were unavailable and void to non-COVID infections. Average bed occupancy remains high at 94.0%, slightly up from last week (93.8%). This is 1.9 percentage points higher compared to the same week last year.
Long stay: The number of patients staying in hospital longer than seven, 14 and 21 days has continued to fall this week, down by 1.5%, 1.7% and 2.3% respectively. However, compared to the same time last year, the numbers of patients staying in hospital for longer than seven, 14 and 21 days have all increased (up by 9.9%, 10.0%, and 8.5% respectively).
Neonatal intensive care beds: Occupancy has increased to 66.9% from 64.8% last week, and down from 70.7% the same week a year before. The average number of care beds open is at 1,702, three beds fewer than last week.
Paediatric intensive care beds: Occupancy has remained similar this week to 81.4% (it was 81.7% last week) and it's the lowest it's ever been this winter. However, this is still higher than the same week last year (74.1%). The average number of care beds open has increased by one to 357.
Respiratory syncytial virus (RSV): An average of 30 paediatric beds were closed this week due to RSV symptoms, slightly down from 31 last week and up considerably from eight last year.
Staff absences: There were an average of 48,485 total absences each day this week, of which 8% were COVID-19 related (3,922). The total number of staff absences decreased from the week before but the proportion of COVID-19 related absences remained the same.
Our view
The data this week reflect the intense demand that trusts are facing; we are still seeing extremely high levels of bed occupancy and ongoing challenges with patient flow. However, data from the ambulance sector is encouraging. Despite the number of arrivals to A&E remaining high, this week has seen another decrease in hours lost due to handover delays. This highlights the focused work of trusts across the country in the face of record high staff vacancies and escalating strike action.
Furthermore, other encouraging figures can be observed in the number of G&A beds occupied by flu patients, which continued to decrease this week, suggesting a slight alleviation of pressure arising from seasonal illnesses. Nonetheless, system wide challenges persist, and although this year has seen increases in the number of beds open, G&A bed occupancy remains concerningly high, as does the number of medically fit patients remaining in hospital (59.5%), a symptom of system wide challenges across health and social care.
A new facility improves diagnostic access in north and east Cornwall
Debbie Richards, chief executive at Cornwall Partnership NHS Foundation Trust and Steve Williamson, chief executive at Royal Cornwall Hospitals NHS Trust discuss their new diagnostic centre which is helping to improve diagnostic access.
Autumn 2022, saw the opening of the first phase of a new community diagnostic centre in Bodmin; housing the county's fifth CT scanner and the first to be located east of Truro.
Just months after its opening, the centre has contributed to a reduction in waiting times, elective recovery, and referral to treatment targets. So far over 600 CT scans, 1,350 MRIs and 300 ultrasound scans have been delivered. In May 2022 there were over 58,000 people on a waiting list in the local system. 
The additional diagnostic facilities, which will predominantly benefit people living in north, east and mid Cornwall is located alongside one of the county's community hospitals. This approach is in line with the diagnostic strategy to move such services away from busy acute hospital sites. It is also aligned with the philosophy to provide more care closer to home, reducing travel time and costs, and creating local jobs.
A true NHS partnership, the management and redevelopment of the building has been led by Cornwall Partnership NHS Foundation Trust while the clinical imaging team is employed by the Royal Cornwall Hospitals NHS Trust.
Emma Spouse, diagnostic imaging lead at Royal Cornwall Hospitals NHS Trust, said:
"It is making a real difference to patients to have access to CT and MRI services in the east of the county. The centre provides a calm, outpatient scanning environment that also alleviates our hard-pressed acute and emergency diagnostic imaging services in Truro. Digital technology and connectivity ensure expert advice and opinion is immediately available to the Bodmin Community Diagnostic Centre clinical staff, supporting our services on this site to meet exemplary standards.
"Our thanks go to professor Sir Mike Richards for his national vision to provide more diagnostic services in local communities where people live, to NHS England for funding this excellent new facility, including the top of the range digital x-ray equipment and a new CT scanner, and to the estates team at Cornwall Partnership NHS Foundation Trust who have worked tirelessly with the sub-contractors, our clinical teams and the equipment providers, GE and Philips, to transform the old building into a clinical hub that focusses on rapid diagnostics and onward treatment. It is a fantastic new facility for patients and for the staff who work here."
This is phase one of a three-phase scheme, using early adopter funding which was secured by the Cornwall and Isles of Scilly Integrated Care Board. Phase one, which is fully operational includes CT, X-ray, ultrasound and two hard standings capable of hosting hospital to mobile imaging trucks of any modality.
Phases two and three will be completed later this year. These will see the development of an urgent treatment centre, with the relocation of minor injury unit staff from the neighbouring community hospital. Phase three, the final phase will see the second floor turned into a multi-use clinical space which will fulfil the outstanding community diagnostic facilities.
When fully operational, the centre will deliver an additional 120,000 diagnostic tests per year, helping to support the achievement of national diagnostic waiting time targets. The Bodmin Community Diagnostic Centre will help to relieve pressure on the Royal Cornwall Hospitals NHS Trust, University Hospitals Plymouth NHS Trust as well as trusts further afield in Devon, offering mutual aid, urgent care and wider patient choice.