

This week as the temperature drops and cold weather continues, we review both week 10 of the sitreps and the monthly performance figures – both show a system responding to increased demand across all services.
There were 2mn attendances at A&E in January, an increase of 5.5% compared to the same time last year. A similar proportion (85.3%) of patients attending were seen within four hours, despite there being over 100,000 more attendances than last year. Performance against the A&E 4-hour target is slightly better than this time last year but four out of five trusts are still unable to meet the 95% target.
In January, after the decision to admit, the figures for those waiting longer than 4 hours and 12 hours to be admitted is the highest on record.
Bed occupancy rates seem to be fixed around 95% for the whole of January but the average long stay over 21 days is the highest it has been all winter this week. However, the focus on reducing the number of delayed transfers of care seems to be working with the average number of delayed beds falling from 6,305 last December to 4,688 this year. This is the lowest since August 2015 and efforts from both the NHS and social care have contributed to this improvement.
The focus on reducing the number of delayed transfers of care seems to be working with the average number of delayed beds falling from 6,305 last December to 4,688 this year. This is the lowest since August 2015 and efforts from both the NHS and social care have contributed to this improvement.
As the delayed transfers of care continue to fall, it is possible that the increase in long stays of over 21 days is a result of increased acuity and dependency, simply meaning patients are more seriously ill and need more care and treatment.
In addition, the increase in calls to NHS 111 compared to last year shows that the demand from the public is increasing the use of all services across the system and people are not only attending A&E.
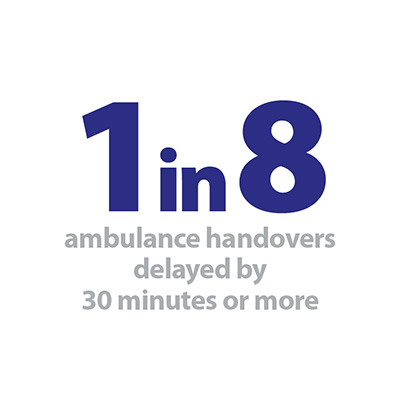
Ambulance services have been under immense pressure again this week with the number of diverts remaining relatively high at 36. Many patients continue to face long delays as they are handed over from ambulances to A&E with 1 in 8 handovers being delayed by 30 minutes or more. Since the start of winter nearly 30,000 people have had to wait more than an hour.
You can find out more about what the data means in our new explainer and download our winter sitrep dashboard to see the figures in more detail.
As the delayed transfers of care continue to fall, it is possible that the increase in long stays of over 21 days is a result of increased acuity and dependency, simply meaning patients are more seriously ill and need more care and treatment.
Insight from the frontline
This week, Wayne Bartlett-Syree, director of strategy and sustainability at East of England Ambulance Service NHS Trust describes how interdependencies and pressures across the whole health and care system, uniquely impact on the ambulance service.
Under the spotlight
It is no surprise that the period between Christmas and the first week of January was incredibly challenging. The trends nationally are that people are sicker and demand continues to increase. Year on year the NHS is finding it harder to meet the rising tide of demand against a constrained pot of money. We are one flu epidemic or significantly cold winter away from the NHS not being able to cope. The urgent and emergency care system is at times in the equivalent position of trading on the edge.
The consequences of this are conveyed powerfully in a recent video published by NHS England, which sets out the risk to patients in the community when systems do not effectively manage and reduce handover delays. As an ambulance trust we and, more importantly, our patients are now having to face the reality of this risk with our NHS partners.
It is now commonplace over the winter period for A&E corridors to become full of patients and ambulances to queue outside emergency departments. It means that patients in the community could be having heart attacks and strokes when there are no ambulances available to provide an emergency response. The risk of harm is now transferring from those in corridors to patients in the community needing an ambulance.
There is plenty of learning from this winter for us as a trust, which we must and will act upon. Monitoring feedback from our staff, patients and their families is important in helping us understand risks and, where necessary, reduce harm.
Director of strategy and sustainability at East of England Ambulance Service NHS Trust
From an ambulance perspective working across six STPs, we can see where systems are coming together and working to keep patients safe. However even those considered best in class are finding it impossible to deliver on the 4-hour A&E waiting time targets. Previously, the 4-hour target was the central measure of system success or failure. The measure of the bottleneck has now extended from inside the emergency department to the forecourt and the ambulance bays outside. Handover delays are probably now a better measure of systems being able to cope with the demands being placed upon them.
What we have experienced over winter is symptomatic of whole systems being under intense pressure. As a service, we are a part of those systems and there are many points at which failures might occur.
For the last few weeks, our trust has been criticised in parliament for potential harms and deaths that might have occurred because of delays in ambulance responses.
Our job is to make sure we give the sickest people the best care possible, and we all feel a deep sense of remorse when any patient does not get a high standard of care. Professionally, our staff feel incredibly distraught that patients may have been harmed.
There is plenty of learning from this winter for us as a trust, which we must and will act upon. Monitoring feedback from our staff, patients and their families is important in helping us understand risks and, where necessary, reduce harm. Along with the executive team, I have listened to staff and their anxieties. That is why we champion the Freedom to speak up approach that allows concerns to be raised safely and – if need be – anonymously. Of the utmost importance for any organisation is the next step in that process – that our leaders set out clear actions to make lasting change.
Exceptional pressure on NHS continues but notable improvements in delayed transfers of care
Responding to the latest data, Saffron Cordery, director of policy and strategy and deputy chief executive at NHS Providers, said:
"These figures show there has been absolutely no let-up in the pressures on the NHS. As always the biggest priority for NHS trusts and staff is ensuring patient safety. They are working flat out, often in extremely challenging conditions.
"While A&E departments remain under significant pressure, NHS trusts across the country have managed to not let performance against the four hour A&E target slip below what it was last year. That is despite there being over 100,000 more attendances to A&E departments this January.
"It is also a concern that many patients continue to face long delays as they are handed over from ambulance to A&E. Since the start of winter nearly 30,000 people have had to wait more than an hour.
"Bed occupancy remains well above recommended safe levels, but the positive news is that fewer patients are facing delays in being transferred out of hospital once they are medically fit to be discharged. Dealing with this has been a big priority for NHS trusts and local councils working in partnership over the winter and it is paying off for patients.
"More generally, these figures are another clear sign of a system that is overstretched. We know the worst of winter may be yet to come. Continuing cold weather will inevitably add extra strain to services which are already struggling to cope. All of this points to the need for a long-term funding settlement for the NHS and social care to be reached – one that enables local care services to deliver the standards that patients deserve."