
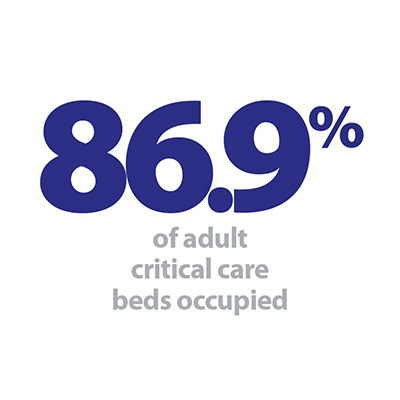
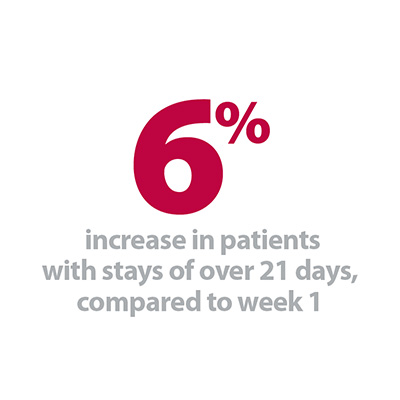
This weeks’ winter sitreps feel like a tale of two halves. There is no doubt that overall the figures show an NHS which is extremely challenged, and still reeling from the high demand of the past two weeks. The number of beds occupied by long stay patients is the highest it has been this winter, occupancy of general and acute beds remains high at an average 94.9%, average occupancy of adult critical care beds was 86.9%, the highest so far this winter, and the number of hospitalisations for flu remains firmly in Public Health England’s 'very high impact' bracket. However there are signs of stabilisation: at just six the number of A&E diverts is the lowest it has been this winter, the number of open escalation beds has started to go down, and the percentage of ambulance handovers delayed by 30 minutes or more has reduced by almost 4 percentage points in just one week.
You can find out more about what the data means in our new explainer document and download our winter sitrep dashboard to see the figures in more detail.
An important part of the week was talking to patients about how they felt their care was going. They told us some amazing and positive stories about how caring our teams are. However, they also challenged us to improve in areas such as the timeliness of medications to take home. There is more we can do.
Chief Operating Officer, Yeovil Hospital NHS Foundation Trust
Simon Sethi, Chief Operating Officer at Yeovil Hospital NHS Foundation Trust, tells us about the challenges they have faced over the past few weeks but also how staff have worked hard both to plan for and recover from these challenges:
"We’ve been on a journey over the last two years to improve patient experience, reduce length of stay, and make our hospital an enjoyable place to work despite the challenges seen across the NHS. This started after a very challenging winter featuring routine escalation, elective cancellations, and staff burn out. Through a focus on ambulatory care, integration with primary care, relentlessly reducing patient waits in hospital, and working with social care to get people home sooner, we’ve seen significant improvements. Length of stay has dropped 10%, we’ve achieved the four hour standard for 12 months, and staff are increasingly keen to join the hospital as it becomes a more enjoyable place to work."

"However, as with all NHS teams at this time of year, Yeovil Hospital is seeing high demand, acuity, and seasonal viruses that challenge us to maintain the standards of care our patients expect. Activity at our emergency department is 14% higher than last year and we’ve faced the challenge of controlling Norovirus outbreaks that are difficult to avoid given its presence in the community. One key change we’ve seen this year, particularly when we declared OPEL 4 after New Year, is the support of partners. When we raised serious concerns about our ability to cope, the community helped with more beds, social care ensured no delays, and acute partners offered support. This camaraderie in the face of the challenges we all face makes a huge difference.
As part of our plan to recover the site last week we ran our iCARE About Patient Time week which aimed to ensure every patient in the hospital receives the diagnosis and treatment they need as soon as they need it. We partnered Matrons and Managers with each ward to reduce delays for patients, increased ward rounds, and ran Director and Clinical Director walk-arounds every day to talk to wards about how they’re finding things and how we can help. We also ran daily competitions with hampers which always goes down well!
An important part of the week was talking to patients about how they felt their care was going. They told us some amazing and positive stories about how caring our teams are. However, they also challenged us to improve in areas such as the timeliness of medications to take home. There is more we can do.
Despite all these actions we remain in a challenged position and a question for me is how we ensure the constant focus on flow and minimising delays is sustainable for our teams. We’re actively working with primary care, clinical teams, and our community partners to ensure we can maintain good and sustainable care at such challenged times."
When we raised serious concerns about our ability to cope, the community helped with more beds, social care ensured no delays, and acute partners offered support. This camaraderie in the face of the challenges we all face makes a huge difference.
Chief Operating Officer, Yeovil Hospital NHS Foundation Trust
Responding to today’s figures, NHS Providers director of policy and strategy, Saffron Cordery, said:
"These figures show conditions remain extremely challenging.
"Although we saw a very slight easing of pressures last week, NHS trusts are still working at or beyond full stretch, resulting – at times – in care for patients that falls short of what trusts and their staff want to provide.
"Having said that, it is encouraging to see how NHS trusts have worked to recover the situation, with far fewer ambulance diverts and a significant drop in delays to hand over patients when they arrive at A & E.
"However bed occupancy rates are still almost 10 per cent higher than the recommended safe level of 85 per cent, and it is worrying to see the figure for adult critical care beds at the highest level so far this winter.
"The impact of flu and cold weather remain a serious concern. The worst of winter may be yet to come.
"It is clear we have reached a watershed moment.