

This weeks’ winter sitrep data has been the most highly anticipated yet, with stories of the winter pressures facing trusts in the media well before the data was released.
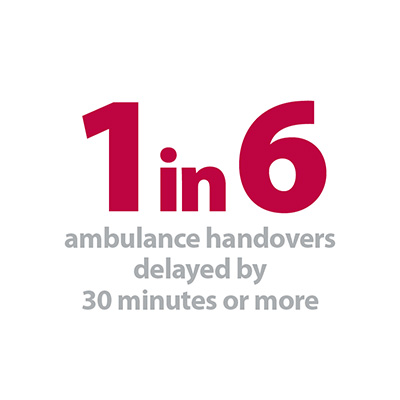
The most striking data in this weeks’ release is for ambulance arrivals and delays. The 137 reporting trusts received 97,706 ambulance arrivals this week – that’s the equivalent of all 137 trusts receiving an ambulance every 15 minutes, 24 hours a day. Unsurprisingly A&E departments have been overwhelmed by this level of demand and the number of ambulance handover delays (the wait between an ambulance arriving and the patient being transferred to the A&E department) was the highest so far this winter. This week 1 in 6 arrivals were delayed by over 30 minutes and 1 in 20 were delayed by over 60 minutes. This is not a problem isolated to a handful of challenged areas, but is widespread across the NHS with 108 of the 137 trusts (79%) experiencing at least one over 60 minute delay this week.
Many commentators were expecting bed occupancy to have soared this week, and might be surprised to see a weekly average of 91.7%, well below the 95% seen in week three. But, when taking in to account the fact that planned care requiring inpatient stays, such as routine surgery, would have been paused, it is no surprise that levels are lower. Also, when we look at the daily data we can see that while bed occupancy was low on Christmas Day (an average of 86.7% and only 27 trusts reporting occupancy of over 95%) by New Years’ Eve it had increased to 93.5% with 69 trusts (50%) reporting occupancy of over 95%, despite an additional 800 beds being opened during the week.
The most striking data in this weeks’ release is for ambulance arrivals and delays. The 137 reporting trusts received 97,706 ambulance arrivals this week – that’s the equivalent of all 137 trusts receiving an ambulance every 15 minutes, 24 hours a day.
As we highlighted in week 1, the winter sitrep data only provides part of the picture. If anything, the data published this week does not provide the full scale of the challenges facing the NHS over the festive period. It’s not just the demand for NHS services which has been challenging, but also the type of demand - many trust leaders and senior clinicians are reporting to us that they have been seeing sicker and frailer patients, exacerbated by increasing flu, respiratory conditions and norovirus. Flu started to become a significant concern in week five, with more people hospitalised and admitted to intensive care, above the respective baselines from last year.
Some hospitals reported that on some days they were only able to see between 40-60% patients attending A&E within four hours, well below the 95% target and below the standard of care trusts want to provide. The A&E data for December is due for publication next Thursday and we’ll be able to see the impact of this nationally. Although not nationally reported this year, some have suggested that around 24 trusts are on Opel 4 (previously known as a "black alert"), the highest level of escalation within a trust.
As many of us were having a break over the festive period, NHS frontline staff were working flat out to provide high quality care to patients in really difficult and pressurised circumstances, among them this weeks’ NHS winter heroes.
It’s not just the demand for NHS services which has been challenging, but also the type of demand - many trust leaders and senior clinicians are reporting to us that they have been seeing sicker and frailer patients, exacerbated by increasing flu, respiratory conditions and norovirus.
Winter heroes
NHS staff across the health service, including at North Bristol NHS Trust, have taken the initiative to keep services running in response to winter pressures, for example by switching from their usual roles to support emergency care colleagues, or collecting patients rather than waiting for a porter to be free. The trust says its porters, who are particularly busy at this time of year, receive regular compliments from patients. Robert Weedon, who has been at the trust for 40 years, has a "smile and a kind word for everyone".
There are many more examples of staff going the extra mile, including the nurses from the East Cheshire NHS Trust safeguarding team whose willingness to step in at a weekend to assess people at a residential care home under threat of closure helped it to remain open.
A physiotherapist at Newark hospital – part of Sherwood Forest Hospitals NHS Foundation Trust – came in at 4:30am to assess and advise a patient on getting out of bed to use her commode – which meant she could be discharged on the planned day.
And a senior nurse in a busy community learning disability service at Southern Health NHS Foundation Trust worked extra hours – even while covering for vacancies in her team - to support a service user who was terminally ill and her carer family, until she died peacefully at home shortly before Christmas.
NHS Providers reaction
Responding to the latest NHS England winter performance figures, the director of policy and strategy at NHS Providers, Saffron Cordery said:
"The figures reflect what we are hearing from the NHS front line that despite planning more meticulously than ever before, the level of demand for services means severe pressures remain across the health and care system.
"Overall bed occupancy remains well above recommended safe levels, but would almost certainly be significantly higher without the extensive preparations put in place to deal with winter pressures. Ambulance services are under strain with delays at high levels, and 39 A&E diverts in place this week. This coupled with the highest number of ambulance arrivals this winter has a knock on effect for A&E departments.
The health service must focus first on those patients who need help most, though we recognise the inconvenience and distress this will cause for many people whose procedures will be delayed.
"NHS trusts are telling us that respiratory problems, flu and norovirus are making an impact. This mixed with GPs under real pressure creates serious problems for trusts.
"This is why we welcomed sensible and proportionate recommendations from the National Emergency Planning Panel. The health service must focus first on those patients who need help most, though we recognise the inconvenience and distress this will cause for many people whose procedures will be delayed.
"Although these measures will help keep patients safe in the short-term, it will have an impact on the service's ability to meet waiting time targets. We must square this circle as part of a longer-term plan which is realistic about what the service can deliver with the funding and resources available. We must learn lessons from this winter."