

After eight weeks of reporting sustained pressure at the frontline through winter watch, there are still only some signs of stabilisation in this week’s data. The impact of day-to-day relentless pressure and this level and type of demand places on services should not be underestimated, with staff across the NHS having to go the extra mile to care for and treat patients quickly and safely.
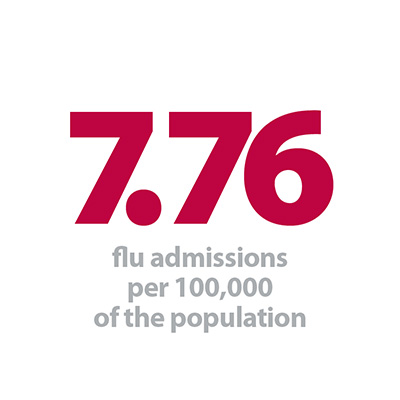
Key pressure points such as ambulance handover delays and flu are starting to ease a little. Demand for ambulances was down to the lowest level so far this winter, with handover delays over 60 minutes down to 2.4%, compared to 2.8% last week. As we have seen over winter so far, long ambulance delays are an important indicator of whole-system pressure so the trend is starting to head in the right direction. Flu hospitalisations have decreased from their highest point last week, and there has also been a reduction in admissions to intensive care.
But frontline services are still facing substantial capacity constraints. The number of beds closed to norovirus increased again this week, up to 742, which has implications for bed availability. Bed occupancy remains persistently high, at an average of 94.8% of general and acute beds occupied, only marginally down from last week’s peak this winter. Only four trusts (out of 137 reporting) had occupancy levels below the 85% recommended level.
You can find a detailed breakdown of how this week compares to the rest of winter in our dashboard.
This week, we asked communications leaders at our network event what the biggest challenges in communications posed by the added winter pressures have been:
Frontline staff are working around the clock to treat patients safely and quickly, to ensure that there is enough capacity to meet demand. This is why trust efforts to maximise existing resources are so important. In this week’s blog, Paula Shobbrook, director of nursing and midwifery and deputy chief executive, The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust, shared her reflections on running a ‘perfect week’ this winter:
“At Royal Bournemouth and Christchurch Hospitals (RBCH) we started a quality improvement week in January by asking our staff: “What would make this week perfect for you and your patients?”
The week aimed to rapidly improve our bed situation and to help us meet the four-hour waiting time target in our A&E. Over 50 issues were escalated to the hub in the major incident room, and around two-thirds of these were resolved during the week. Many of our trust’s senior leaders and clinicians were out and about, helping to resolve issues. Peter Gill, our IT director, was paired up with the discharge team and managed to resolve IT compatibility and database issues which people had, as he said, “suffered in silence” with for years.
We also gave staff permission to try ideas to improve processes, with support from our quality improvement team. We use the plan-do-study-act (PDSA) cycle approach, which is a scientific method of testing improvement ideas.
Director of Nursing and Midwifery and Deputy Chief Executive, The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust
We also gave staff permission to try ideas to improve processes, with support from our quality improvement team. We use the plan-do-study-act (PDSA) cycle approach, which is a scientific method of testing improvement ideas. We ran with over 25 ideas; many succeeded well, but we also learned from those which did not. When we reviewed them at the end of the week, we determined 27 actions across nine broad themes. We allocated each action at the debrief meeting so it is clear who is taking them forward. As many as possible are “just do it” actions as we know the importance of rapid adaptation in the current climate.
An example of a successful PDSA test was that the advanced nurse practitioners worked different hours in the acute medical unit so they could cover evenings and the weekend, and bed space was set aside during daytime hours to enable them to assess patients with more confidentiality and dignity. It was agreed to continue this way of working into the future.
The daily tempo was high, with four short meetings per day. Regular bed meetings were held at 10am and 2pm, but were moved to the major incident room to give greater urgency; extra meetings were held for staff to report or resolve issues at 12pm and 4pm. We gained valuable input and learning from our partners such as community matrons, social workers, and GPs. We also shared our learning with Poole Hospital, and jointly featured in a primetime breakfast show live on BBC Radio Solent.
Our A&E performance improved. The mean time spent in A&E by patients who were admitted fell significantly to 3hrs 45mins (previous weeks 4:38, 5:00, 4:28, 4:52, 4:10). This is a good reflection of improved flow through the whole hospital. We ended the week with nearly 50 beds ready for the weekend, and our A&E performance moved from bottom three to top three for the south of England by the end of the week. This meant that patients were safely cared for in appropriate areas rather than kept waiting in admission areas.
Our cultural shift towards openness over recent years was reflected in our confidence in holding discussions with our regulators (NHS England and NHS Improvement) in the room at various points. They noted the honesty and enthusiasm in our approach.
Director of Nursing and Midwifery and Deputy Chief Executive, The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust
Our cultural shift towards openness over recent years was reflected in our confidence in holding discussions with our regulators (NHS England and NHS Improvement) in the room at various points. They noted the honesty and enthusiasm in our approach. As our director of improvement observed, “We were together having a conversation. Change happens through people”.
Some of our observations on running a “perfect week” would be:
- Try your ideas – a week is long enough to indicate whether most will work or not.
- Keep the tempo up – it was hard work having four meetings per day, but worth it.
- Don’t rely just on emails and internal bulletins. Go around wards with a trolley full of sweets and pens, and get talking to staff!
- The combination of rapid senior decision making coupled with an improvement ethos is explosive."
Responding to today’s figures, NHS Providers head of analysis, Phillippa Hentsch, said:
"These figures show the NHS is continuing to work at, and in some places, beyond its limits. This has been the case since early December.
"Bed occupancy rates are well above recommended safety levels, with persistently high numbers of long-stay patients. That makes it much harder to cope with additional pressures such as flu and norovirus, and can lead to delays for patients who need to be admitted. The rise in ambulance diverts is a further sign of a service that is struggling to cope with demand.
"Trusts and NHS staff are doing all they can to ensure safe, high-quality care in extremely challenging conditions.
"The reality is we have reached a watershed moment where the NHS can no longer deliver what is expected of it under existing funding. We need a long-term funding settlement for health and social care. Planning for these big decisions should be put in train without delay."