
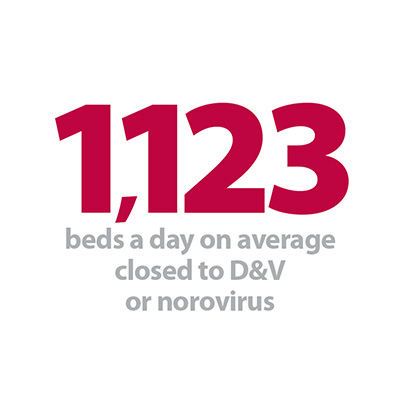
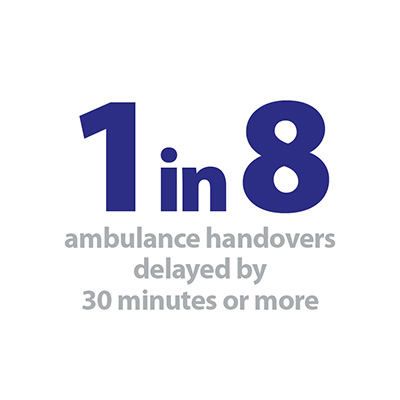
As we start to settle into the new rhythm of winter this weeks’ winter sitrep report shows many measures are stable compared to last week (bed occupancy levels, ambulance arrivals and the number of long stay patients), but with a few hints at increasing pressure and perhaps indications of the start of the cold weather. Last week the number of ambulance diverts increased, ambulance handover delays increased slightly, and, perhaps most notably, the number of beds closed to D&V/norovirus like symptoms almost doubled.
Mark Mould, chief operating officer at Poole Hospital NHS Foundation trust, reflects on the impact this had on their hospital, as well as their ‘Perfect week’ and the newly announced winter funding:
“I love my job, although there hardly seem to be enough hours in the day to fit in all that we do, these busy times of year just highlight how wonderful our staff are. Last week was our 'Perfect patient pathway week', an opportunity for us to focus on making a range of clinical pathways even more efficient and to support patients to leave hospital in a timely way. While the hospital has been very busy, staff across many specialities have been targeting a number of key actions, including reducing the time between request and diagnostic test time for stroke patients, using the nurse-led medical investigations unit (MIU) as an alternative to admitting some patients to a ward bed, reinforcing the need for effective, regular board rounds and adherence to the SAFER patient flow bundle, and identifying ways in which the pathway for patients with fractured hips could improve. Even at these busy times I marvel at the level of passion, commitment and talent displayed by our staff across the organisation and the wider system.
I love my job, although there hardly seem to be enough hours in the day to fit in all that we do, these busy times of year just highlight how wonderful our staff are.
Chief operating officer at Poole Hospital
Generally, staff reported improved communication between teams and services during the week. Staff on MIU avoided a number of admissions, helping patients to get home sooner. There was excellent practice seen at board rounds – I was fortunate to sit in on an orthopaedic board round - while we also launched an updated rapid discharge pathway for patients in the last days of life so they can die at their chosen place.
Locally, our A&E four hour performance across the week was ‘challenged’. Having finished November at 93.13% against an organisational trajectory of 91.05%, last week we tracked at 85% - a level we haven’t experienced recently.
This performance was driven by a number of factors:
- We experienced our first week of norovirus with admissions restricted in a number of ward areas. But more importantly, we were unable to step down those patients who are medically ready to leave hospital unless they were returning home.
- An increase in acuity led to increased bed occupancy and reduced flow throughout the hospital, leading to a lack of availability of assessment beds - the indicator most correlated with four hour performance.
- A significant number of patients were medically ready to leave but waiting for external partners to identify the availability of capacity.
- Medical and nursing vacancies across the trust resulted in extended waits to be seen and delays in clinical decision making. Recruitment in the emergency department has improved but there remain gaps at key times.
Even at these busy times I marvel at the level of passion, commitment and talent displayed by our staff across the organisation and the wider system.
Chief operating officer at Poole Hospital
On Friday morning we called an ‘internal capacity incident’, an internal process that we use in the organisation to re-calibrate the internal capacity of the trust but linking closely with our partners and local commissioners to generate system wide solutions to some of the blockages we were experiencing, and we are positive about improving our performance next week.
In addition to the everyday, last week we spent time pulling together bids across Dorset for the winter monies announced in the budget, and had a number of conversations across the week with national teams on those proposals and the expectations that come with additional investment. Any new money is welcome - the challenge is to make sure that we are spending those monies in the way that gives maximum benefit to patients and staff during the winter period. Our system-wide bids were submitted on Monday and we wait for the national letter outlining the level of funding allocated. Notwithstanding this announcement, we are already implementing local plans in order to have a timely impact this winter.” All in all a very busy week. Whilst there is no doubt we all working under pressure, hopefully our hard work is having a positive impact on the care we provide for our patients.
Poole Hospital NHS Foundation Trust is an acute general hospital on the south coast of England and also the designated trauma unit for East Dorset.
These figures show the NHS is responding well to growing pressure. The health service has prepared more extensively for this winter than ever before.
chief executive NHS Providers
Responding to the latest performance figures and sitrep data from NHS England, the chief executive of NHS Providers, Chris Hopson, said: “These figures show the NHS is responding well to growing pressure. The health service has prepared more extensively for this winter than ever before. These plans are helping to ensure safe, timely care for patients, but the pressures are great and the system is already running at or close to full stretch. Performance against the four-hour target in A & E in November was better than for the same time last year despite a sharp rise in attendances (4.4 per cent) and emergency admissions (4.8 per cent). It was particularly encouraging to see the sharp drop in 12-hour trolley waits (down 76.1 per cent) and delays in transferring patients who were ready to move on (down 15 per cent). But the more recent daily sitrep data gives cause for concern. Average general and acute bed occupancy is running close to 95 per cent, well above recommended safe levels. We also saw a sharp rise in the number of A & E diverts, and an increase in ambulance handover delays. There was also a marked jump in the number of beds closed because of norovirus.”